|
|
|
|
|
|
|
|
Joyce Leader,Johannes Buca Letshwiti,BERNARD STUART,MJ Turner,Martin White,M Kennelly
|
|
|
Ir Med J. 2012 Jun;105(6):180-2
J Leader1, J Letshwiti2, B Stuart3, MJ Turner3, M White4, M Kennelly5
1UCD, Belfield, Dublin 4
2Letterkenny General Hospital, Letterkenny, Co Donegal
3Coombe Women & Infant’s University Hospital, Crumlin, Dublin 12
4Nobber, Co Meath
5Centre for Policy Studies, UCC, Western Rd, Cork
Abstract
We reviewed the outcome of fetal hydronephrosis with a renal pelvic dilatation (RPD) of 4 -7 mm to assess whether a RPD > 7 mm had a higher predictive value for renal pathology. 373 fetuses were diagnosed with hydronephrosis giving an incidence of 2.2%. The male: female ratio was 1.8:1. 5(1.34%) fetuses with antenatal hydronephrosis were diagnosed with Down Syndrome. 299 (91.7%) fetuses with an RPD of 4 – 7 mm had resolved by 34 weeks gestation with 10 (3.1%) having moderate to severe hydronephrosis. The resolution rate for RPD > 7 mm was 60.7%(17) with 11 fetuses (39.3%) requiring long term follow up.
|
|
Introduction
Antenatal ultrasound offers many benefits including detection of fetal abnormalities which may benefit from timely medical or surgical intervention before or after birth. A potential limitation is the false positive rate associated with the parameters used to assess certain abnormalities and the parental anxiety they can cause. Fetal hydronephrosis, a common finding in obstetric ultrasound is one such condition. In our unit, fetal hydronephrosis is defined as an anterior-posterior renal pelvic diameter (RPD) of ≥4mm before 28 weeks gestation and ≥ 8mm after 28 weeks gestation. The antenatal course is highly unpredictable1 but is most commonly physiological and in the majority of cases undergoes spontaneous resolution2. It can, however, be associated with certain pathological entities including vesico- ureteric reflux as well as pelvi-ureteric junction and vesico-ureteric junction obstruction. Ultrasound is the diagnostic modality of choice and hydronephrosis is detected in up to 5.5%3-6 of all scans. Certain markers are associated with an increased risk of postnatal consequences. These include an increased severity of renal pelvic dilatation, oligohydraminos, megacystitis and megaureter7-9. Studies have also shown that there is an increased incidence in those with chromosomal abnormalities with emphasis being placed on Down syndrome2,10,11.
Despite this knowledge, there is a lack of consensus among fetal medicine specialists or robust data to clarify the cut-off measurement of RPD for continuing antenatal and postnatal monitoring in cases of isolated hydronephrosis (no associated renal abnormalities or extra renal abnormalities). The cut-off value should be one with a high diagnostic rate for an underlining renal abnormality and a low false positive rate. This helps to minimise parental anxiety, reduces the number of unnecessary investigations both pre and postnatally, and provides a cost efficient and effective service without missing any significant renal pathology. There is also a lack of agreement on which RPD measurement warrants karyotyping and the postnatal consequences of the antenatal measurements. The aims of this study were to review the outcome of all fetal hydronephrosis cases detected with an anterior-posterior diameter of 4-7 mm before 28 weeks gestation and to assess whether a measurement of > 7 mm had a higher positive predictive value for renal pathology. We also evaluated the incidence of chromosomal abnormalities in this group as a secondary outcome.
Methods
Ultrasound scans preformed between 2008 and 2009 in a tertiary referral ultrasound and fetal medicine unit in a large university teaching hospital were reviewed retrospectively. The Coombe Women and Infants University Hospital is a tertiary referral unit with an annual delivery rate of approximately 9,110 births. Cases with RPD were detected at routine ultrasound for anatomical review at 20-22 weeks or co-incidentally at a growth scan in the third trimester. These scans were carried out by midwife sonographers and consultants in the ultrasound and fetal medicine department on 2D ultrasound scanners. Over the two year period, all cases diagnosed were either unilateral or bilateral isolated fetal hydronephrosis which was defined as an anterior- posterior pelvic diameter with respect to gestation (Figure 1). Cases with multiple abnormal renal abnormalities such as multicystic dysplastic kidney, hydroureter, calyceal clubbing, amniotic fluid or bladder abnormalities were not included in this study. Fetuses with multiple extra- renal abnormalities were excluded from the study. The inclusion criteria for the study was a renal pelvic dilatation of ≥4mm detected before 28 weeks gestation or ≥8mm dilatation after 28 weeks. An anterior-posterior diameter of 10mm was considered pathological and was reviewed by a consultant in fetal medicine at the time of detection. The unit policy for follow up was to review these patients at 34 weeks gestation with the following diagnostic criteria: Mild hydronephrosis 8 mm – 9.9 mm, moderate hydronephrosis 10 – 14.9 mm and severe hydronephrosis ≥15mm. A follow up scan sooner than 34 weeks was organised depending on the measurement at diagnosis and any associated findings.
As hydronephrosis is associated with an increased risk of aneuploidy, this risk was calculated using previous risk of aneuploidies based on maternal age or nuchal translucency when appropriate, as background risk. If the estimated risk was higher than 1: 250, an amniocentesis was offered. The postnatal follow up included ultrasound scans on day 3-5 of life on all babies with a dilatation of greater then 8mm at the 34 week scan. Further diagnostic scans were then requested depending on the ultrasound findings and at the requests of the paediatric nephrologist. If the postnatal ultrasound examination revealed a RPD < 7 mm, follow-up was discontinued. These cases were then classified as postnatal normal. In cases where the RPD was larger or additional findings were revealed, the management was individualised. In such cases, prophylactic antibiotic treatment was given to all newborns.
Results
A total of 373 fetuses out of 18,250 scans performed were diagnosed with hydronephrosis over the two year period giving an incidence of 2.2%. The majority 354 (94.9%) were diagnosed at the 20-22 week scan and 19 (5.1%) were diagnosed in the third trimester after a normal 20-22 weeks scan. There was a male preponderance with 240 (64.3%) cases of fetal hydronephrosis being male and the remaining 133 (35.7%) cases being female giving a male to female ratio of 1.8: 1. There were 5 (1.34%) fetuses diagnosed in the antenatal or postnatal period with Down Syndrome. The mean maternal age was 32.7 years and the mean gestational age at delivery was 39.2 weeks (Range 28.3 - 42.3 SD=2.1). During the same two year period, there were 44 cases of Trisomy 21 delivered, 5 (11.4%) of which had hydronephrosis.
Figure 1: Ultrasound image of fetal hydronephrosis where the renal pelvices are measured.

Flow Chart 1: A representation of the overall breakdown of results into resolved or diagnosed renal pathology for those who had fetal hydronephrosis between 4 -7mm, > 7mm and those diagnosed in third trimester.
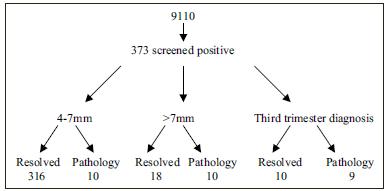
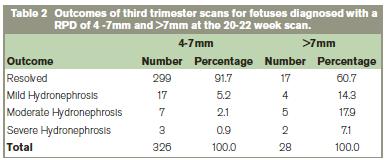
The overall results are depicted in Flow Chart 1. The resolution rate for a RPD of 4-7 mm was high with 91.7% (299 cases) of the entire group having resolved by the 34 week scan. Of those that did not resolve, Table 2 details the outcome.The mean RPD in these cases was 6.5mm. 17 fetuses had an RPD 4mm of which all resolved. Of those diagnosed at the 20-22 week scan, 28 fetuses (7.5%) had a RPD > 7mm. The resolution rate was less in the RPD >7 mm with 17 (60.7%) resolving and 11 (39.3%) requiring long term follow up.Of the 19 diagnosed in the third trimester 9(47.3%) had an underlining renal abnormality. Overall an underlying abnormality / pathology was present in 29 (7.78%), 11 (37.9%) of which were female and 18 (62.1%) male.These cases included: Pelvi-ureteric junction obstruction(8), vesico-ureteric junction obstruction(5), strictures(6), duplex systems(7) and posterior urethral valves(3). These cases required on going long term follow up. Table 2 details the results from the third trimester scans.
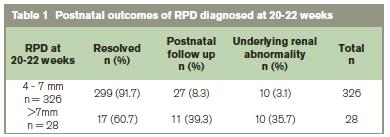
RPD: renal pelvic dilatation
Discussion
Our data highlights the natural course of isolated fetal hydronephrosis (RPD 4-7 mm) diagnosed at 20-22 weeks gestation is of resolution during the pregnancy or the neonatal period. This supports the view that they do not necessarily need a third trimester or a postnatal scan, but 10 (3.1%) cases of possible pathology could be missed. As stated the mean RPD in these cases was 6.5 mm, which may suggest that a 6mm cut off may be more sensitive for a higher detection rate with a low false positive rate. Without doubt, a renal pelvic cut off measurement of 7 mm, has a higher diagnostic rate for renal pathology (35.7% versus 3.1%). As there is a natural history to diseases, one may argue that management may be better informed by repeat examinations and trends and not on single estimates. Our date suggest that a RPD cut-off of 6 mm would increase the detection rate for renal pathology with a lower false positive rate than 4 mm.
The 1.3% prevalence of Trisomy 21 in this group of isolated kidney dilatation, without taking maternal age or any other risk factors into account was higher than expected12,13. However, the unit policy for soft markers at that point, did not include nuchal pad or humerus length, so in fact, this group may include other soft markers and hence not represent isolated hydronephrosis. Regarding the sex distribution, the male preponderance was also reflected in the resolution rate, hence this indicates that female fetuses with renal pelvic dilatation have a higher probability of non resolution and underlying pathology. In summary, this review suggests that a RPD of ≥ 6mm at 20-22 weeks has a high detection rate for renal pathology with a low false positive rate. Ten of the eleven cases with RPD at 20-22 weeks > 7mm were found to have renal pathology in the neonatal period and required long term follow up. The structured antenatal follow up of a 34 week scan enables an assessment of those with progression to be followed up promptly in the neonatal period hence minimising parental anxiety and reducing the number of unnecessary investigations.
Correspondence: J Leader
Apt 1, 91 Harcourt Street, Dublin 2
Email: [email protected]
References
1. Avni FE, Cos T, Cassart M, Massez A, Donner C, Ismaili K, Hall M. Evolution of fatal ultrasonography. Eur Radiol 17: 419-431
2. Langer B, Simeoni U, Montoya Y, Casanova R, Schlaeder G. Antenatal diagnosis of urinary tract dilatation by U/S. Fetal Diagn Ther 1996; 11: 191-198
3. Ek S, Lidefeldt KJ, Varrico L. Fetal hydronephrosis; prevalence, natural history and postnatal consequences in an unselected population.Acta Obstetricia et Gynaecologica.2007; 86:1463-1466
4. Persutte WH, Koyle M, Lenke RR, Klas J, Ryan C, Hobbins JC. Mild pylectasis ascertained with prenatal ultrasonography is pediatrically significant. Ultrasound Obstet Gynaecol 1997;10:12-8
5. Livera LN, Brookfield DSK, Egglington JA, HAwnaur JM. Antenatal ultrasonography to detect fetal abnormalities: a prospective screening programme. BMJ 1989; 298: 1421-3
6. Cohen-Overbeek TE, Wijngaard-Boom P, Ursem NTC, Hop WCJ, Wladimiroff JW, Wolffenbuttel KP. Mild renal pylectasis in the second trimester; determination of cut-off levels for postnatal referral. Ultrasound Obstet Gynaecol 2005; 25: 378-383
7. Olivera EA, Diniz JSS, Cabral ACV, Leite HV, Colosimo EA, Oliveira R, Vilasboas AS. Prognostic factors in fetal hydronephrosis: a multivariate analysis Pediatr Nephrol 1999; 13:859-864
8. Olivera EA, Diniz JSS, Cabral ACV, Pereira AK, Leite HV, Colosimo EA, Vilasboas AS. Predictive factors of fetal urethral obstruction: a multivariate Analysis. Fetal Diagn Ther 2000; 15: 180-186
9. Wollenburg A. Newhaus TJ, Willi UV, Wisser J. Outcome of fetal renal pelvic dilatation diagnosed during 3rd trimester. Ultrasound in Obstetrics and Gynecology 2005; 25: 483-488
10. Ouzounian J, Castro M, Fresquez M, Al-Sulyman OM, Kovacs BW. Prognostic significance of antenatally detected fetal pyelectasis. Ultrasound Obstet. Gynaecol. 1996; 7: 424-428
11. Oluleye Thompson M, Thilaganathan B, Effect of routine screening for downs syndrome on the significance of isolated fetal hydronephrosis. British Journal of Obstetrics and Gynaecology. 1998; 105: 860-864
12. Nicolaides K, Snijders R. Features of chromosomal defects. In: Pilu G, Nicolaides KH, editors. Diagnosis of fetal abnormalities- the 18-23 week scan. The Parthenon Publishing Group Inc;1999.p99-104.
13. Chudleigh PM, Chitty LS, Pembrey M, Champell S. The association of aneuploidy and mild pyelectasis in an unselected population: the results of a multicentre study. Ultrasound Obstet Gynecol. 2001;17:197-201.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|