Abstract
A significant amount of valuable undergraduate medical teaching may be informal, unscheduled and delivered by non-consultant hospital doctors (NCHDs). 800 Questionnaires were distributed to consultants, NCHDs and medical students in Irish teaching hospitals. The aim was to quantify the level of unscheduled teaching carried out in these hospitals and the manner in which it was performed. The response rate was 46% (364/800). 71% of doctors who replied are independently teaching undergraduate medical students (77/109), including 71% of interns and senior house officers (48/68). Students tend to prefer small group teaching. Fifty-six percent of students suggest they would benefit from more surgical teaching time (144/255). No interns surveyed were scheduled to teach as part of a formal curriculum. A significant amount of unscheduled teaching by interns and senior house officers takes place in Irish hospitals. It may prove beneficial to incorporate interns into scheduled surgical teaching curricula.
Introduction
Undergraduate teaching has a powerful effect on medical students, influencing not only grades1, but also career choice2 and enjoyment of surgical rotations3. It has been shown that the level of interest in surgery is declining4 and that resident staff who are effective educators and mentors encourage students to pursue surgical careers2. Teaching is beneficial for house officers as it increases their own medical knowledge5. While carefully constructed curricula are in place, a great deal of surgical teaching is unscheduled and entirely dependent on the consultant or non-consultant hospital doctor (NCHD) involved. These encounters tend to be brief, ad hoc and unplanned6. This informal teaching however, has the potential to have a positive impact on medical students’ experience of surgery. It has been suggested that junior hospital staff are more crucial to the undergraduate learning experience than consultants, as much of the onus of teaching medical students, particularly in the area of perioperative management falls to the NCHDs3.
The present study attempts to quantify the amount of unscheduled teaching provided by surgical NCHDs and consultants in Irish teaching hospitals, and to establish potential for improvement. Interns are in their first year post-qualification, Senior House Officers typically two and three years post-qualification, with Registrars and Tutors typically four to six years and Specialist Registrars greater than five years post-qualification. The secondary aim was to examine the teaching medium with which surgeons and trainees feel most comfortable. The tertiary aim was to assess students’ experiences with unscheduled teaching and to assess their ranking of teachers of different grades.
Methods
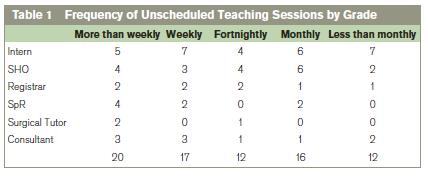
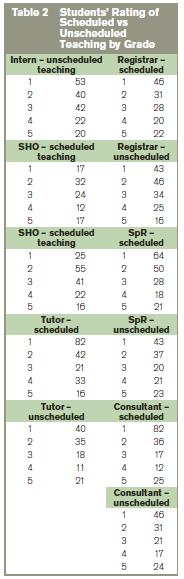
250 questionnaires were distributed over a three month period to NCHDs and consultants working in seven Irish University Hospitals, each a tertiary referral centre with large numbers of undergraduate students attending annually. A total of 550 surveys were distributed to medical students at the end of their training in all major third-level institutions in Ireland. Students were asked to rate which mode of teaching they found to be most useful, again using a 5-point Likert scale with 1 being the most beneficial and 5 being the least beneficial. The modes of teaching investigated were didactic tutorials, bedside tutorials, case presentations, lectures and data interpretation sessions. Following retrieval of the completed questionnaires the results were tabulated and analysed (Tables 1 and 2).
Results
Survey 1
A total of 109/250 (44%) surveys were completed by various grades of hospital doctors - interns (45), SHOs (23), Registrars (10), Specialist Registrars (13), Surgical Tutors (4) and Consultants (14).
Scheduled Teaching
64% (70/109) of responders were not scheduled to provide undergraduate teaching. No intern was scheduled to teach as part of the formal undergraduate curriculum compared to 22% (5/23) of SHOs and 83% (34/41) of registrars, tutors, specialist registrars and consultants. The most common form of scheduled teaching was bedside tutorials 42%, (22/53), followed by didactic tutorials 28% (15/53), with 17% (9/53) scheduled to deliver formal lectures, 11% (6/53) scheduled to hear case presentations and 1% (1/53) scheduled to deliver data interpretation sessions.33% (13/39) responders were scheduled for more than one teaching session per week with 53% (21/39) scheduled for weekly sessions. The remaining 12% (5/39) had been scheduled for fortnightly or less frequent sessions.
Unscheduled Teaching
71% (77/109) respondents provided unscheduled teaching sessions, 64% of Interns (29/45), 83% of SHOs (19/23), 80% of Registrars (8/10), 69% of Specialist Registrars (9/13), 75% of Surgical Tutors (3/4) and 64% of Consultants (9/14) provided unscheduled teaching to undergraduates.The most common mode of unscheduled teaching was bedside tutorials 39% (48/124), followed by didactic tutorials 25% (31/124) and case presentations 24% (30/124). Only a small minority provided unscheduled lectures or data interpretation sessions, 12% (15/124).With regards to frequency of the unscheduled sessions, 64% of responders (49/77) providing unscheduled teaching sessions did so on at least a fortnightly basis (Table 1).
Miscellaneous
33% of (36/109) responders reported adequate time to teach, 33% of interns (15/45), 17% of SHOs (4/23), 40% of registrars (4/10), 38% of Specialist Registrars (5/13) and 35% of Consultants (5/13). 87% surveyed (94/109) could provide fortnightly or more sessions with 14% (15/109) stating they could only teach monthly or less than monthly.75% (39/52) of interns and SHOs reported bedside tutorials (17/52) or didactic tutorials (23/52) as their preferred mode of teaching and 85% reported lectures and data interpretation sessions as the least preferred (44/52).
Survey 2
A total of 184 surveys were fully completed and 71 were partially completed by medical students throughout the country.56% of students felt they were not receiving enough teaching (144/255). 87% felt they would benefit from more scheduled teaching time (221/255). 67% of students (142/255) received unscheduled teaching sessions on a weekly basis and 36% received at least twice weekly sessions (91/255).Students’ rating of scheduled and unscheduled teaching performed by each rank of doctor from intern to consultant is shown in Table 2. 63% of students rated bedside tutorials as the most beneficial mode of teaching (132/184).
Discussion
While the numbers of doctors (109/250) and students (255/550) who replied were less than 50% in both cases this study suggests that in Ireland, a minority of surgeons (consultants and trainees) are scheduled for formal teaching sessions as part of the undergraduate curriculum. These scheduled teaching sessions consist mainly of small group teaching, including didactic tutorials and bedside teaching. The latter was the mode of teaching most preferred by teachers and students alike, but such sessions are limited as only small numbers of students can attend. In order to provide adequate teaching to all students, more tutors are required. The final years of medical undergraduate education are characterised by various in-hospital placements with different specialist teams. This 'clinical apprenticeship' provides opportunities to practice clinical skills under the watchful eye of experienced clinicians who provide constructive feedback and gradually relax their level of intervention as the students become more proficient7. This clinical clerkship is the principal source of mentoring, or form of apprenticeship8.
However, with decreasing numbers of elective surgical admissions9 and increasing numbers of long stay patients10,11, the opportunities for medical students to learn has become more limited. Such long term patients are less suitable for teaching and learning the basics of history taking, physical examination, and clinical evaluation as their acute illness has resolved. Clinical skills are disappearing12, the availability of student mentors has decreased drastically13 and traditional bedside teaching skills have deteriorated as each generation is less exposed to them14. Our study suggests that a significant amount of unscheduled teaching takes place within surgical teams. The junior members of the team are contributing significantly to such teaching and this teaching is valued by the students. Despite this, students feel they are not getting enough teaching in surgery. Small group teaching is the preferred mode of teaching for students and teachers alike and the majority of teachers feel they could commit to fortnightly or greater teaching sessions for undergraduates. Junior members of the surgical team should be treated as a valuable teaching resource as they themselves have experienced final medical exams more recently than any other grade of doctor.
By incorporating interns and SHOs into formal teaching curricula the number of small group and bedside tutorials could increase. Such a policy shift would also increase the number of student mentors available which may augment the clinical skills and expand the medical knowledge of our undergraduate students. In addition, it may upskill teaching skills among future generations, as more students will have augmented exposure to traditional bedside teaching. More regular mentoring may also help to counteract the declining numbers of junior hospital doctors interested in a surgical career15. As interns and the vast majority of SHOs are currently not scheduled to teach, it is reasonable to assume that they could feasibly be incorporated into existing curricula in order to provide extra small group teaching for undergraduates. This should confer greater benefits for both students and teachers alike2,5,6.
Correspondence: D Mulholland
Mater Misericordiae University Hospital, Eccles St, Dublin 7
Email: [email protected]
References
1. Langenfeld SJ, Helmer SD, Cusick TE, Smith RS. Do Strong Resident teachers Help Medical Students on Objective Examinations of Knowledge? J Surg Educ 2011 Sep-Oct;68:350-4.
2. Musunuru S, Lewis B, Rikkers LF, Chen H. Effective Surgical Residents Strongly Influence Medical Students to Pursue Surgical Careers J Am Coll Surg, 2007;203:164-7.
3. Whittaker LD Jr, Estes NC, Ash J, Meyer LE. The value of resident teaching to improve student perceptions of surgery clerkships and surgical career choices Am J Surg 2006 Mar;191:320-4
4. Arnold MW, Patterson AF, Tang L. Has implementation of the 80-hour work week made a career in surgery more appealing to medical students? Am J Surg 2005;189:129–133.
5. Chamberland M, Boulé R. Residents and the teaching role: review of the literature. CMAJ 1990 Oct 15;143:725-30.
6. Jeffree RL, Clarke AC. Ten Tips for Teaching in the Theatre Tearoom: Shifting the Focus from Teaching to Learning World J Surg 2010 34; 2518-23.
7. Ashley EA. Medical Education – beyond tomorrow? Medical Education 2000;34:455-9.
8. Lewis T. The youngest science; Notes of a medicine-watcher. The Viking Press. New York. 1983.
9. Robb WB, O'Sullivan MJ, Brannigan AE, Bouchier-Hayes DJ. Are elective surgical operations cancelled due to increasing medical admissions? IJMS 2004; 173:129-132
10. Costa AP, Poss JW, Peirce T, Hirdes JP Acute care inpatients with long-term delayed- discharge: evidence from a Canadian health region. BMC Health Services Research 2012, 12:172
11. P Gallagher, N O'Callaghan, C Henry. Do Relatives of Elderly Patients Block the Discharge Process? IMJ 2012;105:5
12. Dunnington GL. The art of mentoring. Am J Surg 1996;171:604-7.
13. Mangione S, Nieman LZ. Cardiac auscultatory skills of internal medicine and family practice trainees. A comparison of diagnostic proficiency. JAMA 1997;278:717-22.
14. Ramani S, Orlander JD, Strunin L, Barber TW. Whither bedside teaching? A focus-group study of clinical teachers. Acad Med 2003; 78: 384-90.
15. Erzurum VZ, Obermeyer RJ, Thyagarajan P, Tan P, Koler AK, Hirko MK, Rubin JR. What influences medical students' choice of surgical careers Surg 2000; 128: 253-256.