Introduction
The best practice care for fractured NOF is well-defined. The British Orthopaedic Association provides an evidence-based guideline on management of hip fracture and states that patients should be admitted to an orthopaedic ward within 4 hours of presentation and undergo surgery within 48 hours, if fit. Prompt and effective multidisciplinary intervention can improve quality of care and reduce associated costs.3 At University Hospital Limerick (UHL), we wished to ensure that these targets were met and sought a systems-approach to improving patient flow for those patients presenting to the Emergency Department (ED) with fractured neck of femur. Lean thinking as developed by the Toyota Motor Company incorporates a wide-systems approach to optimising flow of processes, eliminating waste and improving quality. To do this, care is focussed on the patient and how the ‘product’ can be improved to provide a more streamlined, seamless care pathway.
Lean has been used in a number of settings in emergency medicine showing significant improvement opportunities,4 and has been adopted previously in the setting of hip fracture with improvements in mortality for those patients with fractured neck of femur.6 Six-sigma is also a term from industry, developed by Motorola. It seeks to improve the quality of process outputs by minimising variability in production process and by eliminating causes of error. The purpose of this project was to develop and implement a process and controls using Lean and Six-sigma principles to consistently achieve admission within 4 hours and surgery within 24 hours of presentation for all uncomplicated fractured NOF patients. Patients were defined as being uncomplicated if they had an American Society of Anaesthesiology (ASA) score of 2 or less.
Methods
A multidisciplinary project team was assembled comprising representatives from emergency medicine, orthopaedic surgery and operating theatre staff, and from the University of Limerick Lean Healthcare Programme. In order to establish best practice in clinical care of fractured neck of femur, four observational studies were carried out at UHL to establish process mapping of patient management from presentation to theatre. Lean and six sigma concepts were then applied in an attempt to reduce waste and improve upon efficiency. Baseline data regarding all emergency admissions of patients with fractured NOF were collected from May 2008 until December 2010. Collection recommenced during the subsequent trial period, from February to May 2011. Waiting times in the ED and between admission and surgery were recorded.
To study the operational efficiency of the operating theatre, observational information was gathered in orthopaedic theatre by members of the HOPE team on four criteria: the time from request for the first surgical patient of the day from the ward until arrival at theatre, the time of registrar and consultant anaesthetist arrival as well as the time of first patient paint and preparation; the time taken between first patient arrival and commencement of surgery and the proportion of theatre time in which surgery was actually carried out. Data regarding when the first patient from the daily surgery listing actually arrived to theatre was collected from 10 January 2011 until 6 March 2011. Here data collection was limited to Monday through Friday, to give a study period of 40 days.
Once baseline measurements were established, team members identified the following areas for improvement and proposed solutions: 1) The introduction of a fast-track management protocol for fractured NOF to reduce ED waiting times until admission; 2) The improvement of daily theatre times by the introduction of processes to ensure a more timely arrival of first patient to theatre; and 3) Improved communication between all teams involved in patient care. Following this process, observations of ED waiting times, theatre start and usage times and the waiting times for surgery were repeated. Data from pre implementation measurements and post solution development were analysed and compared. All data were analysed using Statistical Package for the Social Sciences (SPSS®) software
Results
ED to Admission
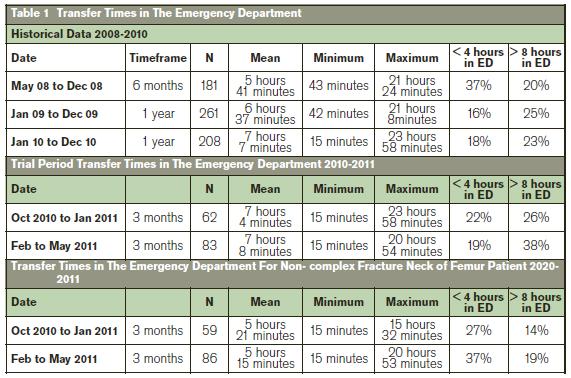
Data collected from May 2008 until December 2010 was grouped and evaluated by calendar year (Table 1). Observational baseline analysis found the mean wait time for a fracture NOF patients to be 7 hours and 7 minutes. The average wait-time in the ED increased by 23% between December 2008 and December 2012. Only 27% of patients were admitted in less than 4 hours. During the trial period of February to May 2011, for all fractured NOF patients the mean wait time in A&E was 7 hours and 8 minutes. Analysis of data specifically for non-complex fractured NOF patients (ASA grade <2) revealed that during the pre-trial period the mean waiting time for admission in the ED was 5 hours 21 minutes with 27% of patients being admitted within 4 hours. During the trial period the mean waiting time for admission was 5 hours 15 minutes with 37% of patients being admitted within 4 hours (Table 1).
Waiting Time until Surgery
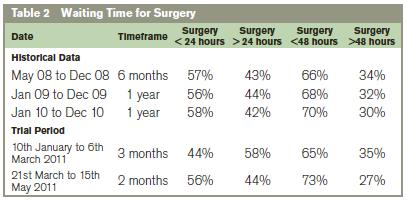
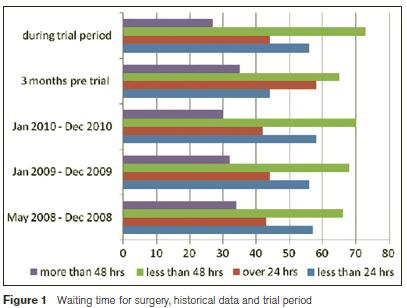
Data collected from May 2008 until December 2010 were evaluated by calendar year. The percentage of all fractured NOF patients who received surgery within 24 hours ranged from 56% to 58% depending on calendar year (Table 2). Analysis of pre-trial data collected from January 2011 until March 2011 reveal that 44% of fractured NOF patients received surgery within 24 hours, 21% received surgery between 24 and 48 hours and 35% received surgery in over 48 hours since presentation (Table 2). Analysis of the data collected during the trial period from March 2011 until May 2011 reveal that 56% of fractured NOF patients received surgery within 24 hours and 27% received surgery in over 48 hours (Table 2).
Theatre Start time
The results of pre-study current state analysis found that between January 2011 and March 2011 the mean start time for the first surgery of the day was 9:10 am and only 3 surgeries beginning before 9:00 am. After protocol introduction, between March 2011 and May 2011 a mean theatre start time was 8:40am, representing a reduction in start time of approximately 30 minutes. During the study period was a reduction in the range of theatre start times from 3 hours and 15 minutes pre-protocol introduction to 1 hour and 20 minutes post protocol introduction.
Theatre Time Usage
Current state analysis found that during an 8 week pre trail period approximately 273 hours were available to surgery. After protocol intervention the available theatre time was found to increase over 45 hours to a total of 319 hours of time over the 8 week trial period. Following the trial to increase theatre operating capacity on 21st March 2011 the percentage of fractured NOF patients that received surgery within 24 hours was 56% with 27% of patients experiencing surgery delays of more than 48 hours. Compared to the Pre-Trial data this shows an increase of 12% of patients receiving surgery within 24 hours and a decrease of 8% of patients experiencing delays of more than 48 hours.
Discussion
Hip fractures are a major cause of morbidity and mortality in the older people.1 This increase will represent a significant strain on the health services in terms of finances, personnel hours and resources used.5 The benefits of proper and prompt treatment of hip fracture have been well established by the British Orthopaedic Association4. This project attempted to design and implement a protocol for the management of non-complex fractured NOF in the UHL to improve efficiency, reduce costs and achieve best practice in care. The most significant impact on the management of non-complex fractured NOF patients noted during this study was the improvement in theatre start time and time usage. The improvements noted in theatre time have several important implications. Firstly, these advances meant that on a consistent basis more patients will be able receive surgical intervention in a timely manner. Secondly, improved time management has implications in terms of cost reduction in healthcare delivery. Finally, these findings support the idea that Lean and Six Sigma principles are tools which can effectively improve the quality of healthcare delivery.
Reducing the amount of time patients stay in hospital has major economic implications. The cost of one night in hospital is €1,3665 and thus increasing the number of patients who are taken to theatre within 24 hours of presentation and thus spending one day less in hospital represents considerable economic savings. During the trial period, there was a reduction of 12% in the number of patients who had to wait over 24 hours for surgery and an 8% reduction in those waiting over 48 hours. Assuming an average of 254 patients per year based on current statistics, and a nightly cost of €1,366, this would yield a projected annual cost saving of €97,149. It is important to acknowledge that there were considerable shortcomings to this project. The target of developing a protocol for non-complex fractured NOF patients to be admitted in less than 4 hours from the time of their presentation to ED was met with only limited success. Overcrowding in ED has been identified as a major contributor to delays and data for this study was gathered during a time at which the ED of UHL was facing periods of exceptionally high delays possibly due to the restructuring of local catchment areas.
In addition it is possible that there was a significant ‘Hawthorn effect’ from being part of the project, and that the successes seen may not be sustainable without the additional resources and emphasis on hip fracture that the project generated. These factors may affect the generalisability of our results. In conclusion this case study has shown that Lean methodology is applicable within the Irish healthcare environment. Lean proved an effective method to guide change resulting in an improved journey for the patient, significant workflow gains through placement of emphasis on having the right patient in the right place, at the right time. Future research should focus on expanding the use of Lean and Six Sigma methodology within the Irish healthcare system with a focus on flow improvement and cost reduction.
Correspondence: R McNamara
Emergency Department, University Hospital Limerick, Dooradoyle, Limerick
Email: [email protected]
Acknowledgements
All staff at University Hospital Limerick who were involved in the HOPE process, and the HOPE team from the University of Limerick.
References
1. Dodds, M.K., Codd, M.B., Looney, A. & Mulhall, K.J. (2009). Incidence of hip fracture in the Republic of Ireland and future projections: a population-based study. Osteoporosis International, 20, 2105-2110.
2. National Institute For Health and Clinical Excellence (NICE). (2009). The management of hip fracture in adults. Accessed March 24, 2013, from: http://www.nice.org.uk/nicemedia/pdf/FNFScopeFINAL.pdf.
3. British Orthopaedic Association (BOA). (2007). The Care of Fragility Fracture Patients. Accessed March 24, 2013, fromhttp://www.fractures.com/pdf/BOA-BGS-Blue-Book.pdf.
4. Holden R J.Lean Thinking in EDs: A Critical Review. Ann Emerg Med;2011:57:265-78
5. Irish Centre for Social Gerontology (2007). The Economic Cost of Falls and Fractures in People aged 65 and over in Ireland. Accessed March 24, 2013, from: http://www.hse.ie/eng/services/Publications/services/Older/The_economic_costs_of_falls_and_fractures_in_people_aged_65_and_over_in_Ireland.pdf
6. Yousri T, Khan Z, Chakrabarti D, Fernandes R, Wahab KLean thinking: Can it improve the outcome of fracture NOFpatients in a district general hospital? Injury, Int. J. Care Injured 42 (2011) 1234–1237
