Ir Med J. 2006 Feb;99(2):58-9
Abstract
With the increasing interest in infection and antibiotic resistance amongst the general public, we undertook to assess the knowledge, and understanding of the treatment and prevention of common infections in medical graduates, about to commence their intern or pre-registration year. A multiple choice-type questionnaire, which included 19 questions, was circulated to 199 recent graduates of three Irish medical schools and 108 (54.3%) were returned. Approximately 60% of the questions were answered correctly. However, questions on the use of antibiotics were poorly answered compared with other questions. With changes in the curricula of many medical schools, there is a need for better education on infection and the use of antibiotics as well as more sophisticated and validated methods of assessment.
Sir,
Introduction
There is much interest in Ireland and elsewhere in revising the undergraduate medical curriculum to meet the needs of current and future doctors. In particular, there is increasing emphasis on integrated teaching programmes with less clear distinctions between subjects. It is also considered that many traditional curricula are factually overloaded.
Although curriculum reform is further advanced in the UK than in Ireland, most medical schools are reviewing their own curriculum, and have either changed, or will be changing it in the near future. Consequently, it may be appropriate to review the understanding and knowledge of recent medical graduates in specific areas. We undertook to assess the knowledge, and understanding of the treatment and prevention of common infections, in graduates who were about to commence their intern or pre-registration year.
Methods
A multiple choice type questionnaire was circulated to the recent graduates of three Irish medical schools during induction programmes, prior to starting as interns or pre-registration house officers. Students were asked to tick the most appropriate answer, from a choice of five, for each of 19 questions. This was done anonymously. The answers were entered into a database, matched against what was considered the correct answer and the results collated according to question type and medical school.
Examples of the questions posed included those seeking factual type information, e.g. “what is the commonest cause of community-acquired pneumonia,” questions on the management of infection e.g. needlestick injuries, questions on the choice of appropriate antibiotics for common infections and, finally, questions on preventative strategies in the hospital and in the community. For the purposes of analysis, the questions were categorised into those that were knowledge-based on issues related to infection and microbiology, (8 questions), those that centred on the use of antibiotics or anti-infective agents (5 questions), and those that covered issues of importance in the prevention of infection (6 questions).
Results
A total of 199 questionnaires were distributed, of which 108 (54.3%) were returned. 31 were received from medical school A, 45 from medical school B, and 32 from medical school C. Of the questions answered, approximately sixty percent (59.6%) were answered correctly.
The highest percentage correct response was obtained for a question relating to the treatment of meningococcal meningitis (95.4%) and the lowest correct response was for a question on when isolation could be discontinued for a patient with Clostridium difficile infection, where only 9.3% correct responses were obtained. Other questions for which there was less than a 50% correct response were those questions dealing with, antibiotics for the treatment of urinary tract infection (25%), cellulitis in the community (25%), Neisseria gonorrhoea (22.2%), hepatitis B vaccination (25%), and the treatment of malaria caused by Plasmodium falciparum (21.3%).
 |
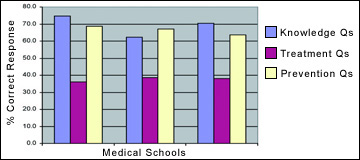 |
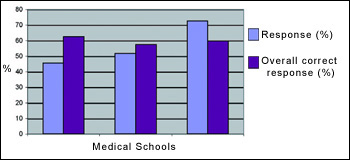
Figure 1 Overall % response and %
correct response for the 19 questions in
the three medical schools
|
Figure 2 Percentage correct responses for
knowledge -based questions, questions
based on the use of antibiotics to treat
infections and question based the
prevention of infection for the three
medicals schools |
Details on the percentage response in each of the three medical schools with the overall correct score, and the percentage correct response in the three categories of questions, are outlined in Figures 1 and 2. Questions on the treatment of infection with antibiotics were poorly answered compared with the other two categories of questions (Figure 2).
Discussion
There is increasing interest amongst the general public, which is reflected in the lay media, on matters relating to infection, especially concerning antibiotic resistance and the use of antibiotics. In Ireland, the Strategy for the Control of Antimicrobial Resistance in Ireland (SARI), launched in 2001 highlights education as an important component of prevention.1 This includes programmes for all clinical professional groups and should clearly start at the undergraduate level for medical doctors. However, understanding the appropriate use of antimicrobials as an undergraduate without prescribing experience is difficult, and this may partly explain the relatively low percentage of correct answers for those questions in this study that were assessing the appropriate use of antimicrobial agents. Most interns or pre-registration officers would be prescribing antibiotics under supervision after qualifying.
Although this survey provides some interesting baseline data on issues that need to be highlighted at the undergraduate and postgraduate level, it has a number of flaws. There was a relatively poor response rate (we may have received responses from the more motivated and knowledgeable student) and the questionnaire did not take cognisance of the differences in the curricula between the three medical schools or how teaching is delivered. It was not possible, for logistical reasons, to follow recent recommendations and guidelines on the designing and distribution of a questionnaire.2,3 Ideally, such a questionnaire should have a higher response rate, the questionnaire should be tailored to the particular curriculum, and the questions should assess factual knowledge and the capacity of the student to analyse data. Furthermore, this type of survey should be repeated at the end of the intern or pre-registration year to see, whether additional clinical experience has lead to significant changes in factual knowledge or clinical judgement.
In the UK, the British Society for Antimicrobial Chemotherapy has an undergraduate education working party which has identified generic learning outcomes for prudent antibiotic prescribing, including clinical skills, patient investigation, patient management, etc.4 A recent survey of antibiotic knowledge amongst 52 final year medical students based at a district general hospital investigated the knowledge amongst those students of proprietary and non-proprietary brand names, emerging and increasingly important antibiotic resistant organisms, and the approximate percentage of patients receiving antibiotics in their hospital at any one time.5 Surprisingly, the students overestimated the proportion receiving antibiotics; 40% believed that 71-100% patients received antibiotics compared with the actual figure of 33% of patients.5
There is a need for a more sophisticated approach to assessing the knowledge and skills that medical students should have in both the diagnosis and management of infections. This will ensure appropriate management of common infections, and provide reassurance to the public who are increasingly concerned about infection, and in particular about acquiring antibiotic resistant pathogens. New curricula must be accompanied by validated methods of assessment, which reflect the quality of the teaching and learning programme, and not just whether students have passed or failed an exam.
Acknowledgements
We wish to acknowledge the help and assistance of Denise O’Mara, Terri Goulding and Dr Bartley Cryan. We also wish to thank all those recent graduates who participated.
H Humphreys1,2, T Dillane1, B O’Connell3, LC Luke4
1Department of Clinical Microbiology,
Royal College of Surgeons in Ireland, Dublin 2
2Department of Microbiology, Beaumont Hospital, Dublin 9
3Department of Microbiology, St James’s Hospital, Dublin 8
4Postgraduate Medical Education Service,
Cork University Hospital, Wilton, Cork
Correspondence: Hilary Humphreys
Department of Clinical Microbiology,
RCSI Education and Research Centre,
Smurfit Building, Beaumont Hospital,
PO Box 9063, Dublin 9
Tel: 00-353-1-809-3708/3710
Fax: 00-353-1-809-3709
Email: [email protected]
References
- Report of the Sub-Group of the Scientific Advisory Committee of the National Disease Surveillance Centre. A Strategy for the Control of Antimicrobial Resistance in Ireland. April 2001.
- Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. Br Med J 2004; 328: 1312-5.
- Boynton PM. Administering, analysing and reporting your questionnaire. Br Med J 2004; 328: 1372-5.
- L.A. Paterson Davenport, Davey PG, Ker JS, on behalf of the BSAC Undergraduate Education Working Party. An outcome-based approach for teaching prudent antimicrobial prescribing to undergraduate medical students: report of a working Party of the British Society for Anti-microbial Chemotherapy. Journal of Antimicrobial Chemotherapy 2005; 56: 196-203.
- Wright EP, Jain P. Survey of antibiotic knowledge amongst final year medical students. J Antimicrob Chemother 2004; 53: 550-1.