|
|
|
|
|
|
|
|
James C Forde,KM O'Connor,DM Fanning,M Guiney,R Grainger
|
|
|
Ir Med J. 2012 Mar;105(3):87-8
JC Forde, KM O'Connor, DM Fanning, MJ Guiney, R Grainger
Department of Urology, St James’s Hospital, James’s St, Dublin 8
Abstract
Endoscopic percutaneous resection of a renal pelvis transitional cell carcinoma (TCC) is a viable treatment option in those who would be rendered dialysis dependent following a nephroureterectomy. We report endoscopic percutaneous resection of an upper tract TCC recurrence in a single functioning kidney followed by antegrade renal pelvis BCG instillation with novel placement of inflated angioplasty balloon in the ureter to help localise its effect.
|
Introduction
Local endoscopic resection of transitional cell carcinoma (TCC) of bladder followed by adjuvant intravesical chemotherapy is very common and routine. For TCC of the upper renal tract this approach is less common with endoscopic percutaneous resection a viable treatment option in those where nephroureterectomy is contraindicated.
Case Report
A 75 year old female previously underwent a radical cystectomy and ileal conduit diversion for TCC of the bladder staged as multifocal pT1 G3 disease. Two years later a surveillance scan suggested of interval development of a urothelial tumour in the left renal pelvis (Figure 1). Longstanding hydronephrosis of the right kidney was again noted that previously had been investigated with a nephrostogram showing no evidence of a stricture or filling defect. An isotope renogram study demonstrated a hydronephrotic non-functioning right kidney.
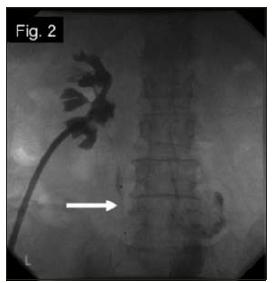
It was decided to endoscopically percutaneously resect the lesion helping to preserve renal function. After left nephrostomy placement, a superstiff guidewire was inserted down the ureter into the ileal conduit. The percutaneous tract was dilated up to 30 Fr and tumour in the renal pelvis was resected macroscopically using a 24 Fr resectoscope with a 20 Fr Malecot catheter placed at the end. Histology confirmed invasive high grade urothelial carcinoma staged as pT1 G3. The Malecot catheter was replaced with a nephrostomy 5 days later. One ampoule (81mg) of BCG (Medac, Hamburg, Germany) was diluted in 50ml of normal saline and instilled through the nephrostomy. To localise its effect, a 4cm by 8mm angioplasty balloon (Wanda, Boston Scientific, MA, USA) was inserted into the mid left ureter (Figure 2) under fluoroscopy. This was inflated with water up to a maximum pressure of 15 atmospheres prior to each instillation to occlude the ureter and deflated after 1 hour. The angioplasty balloon was removed after 6 weekly courses of BCG. A nephrostogram at the time of balloon removal showed no evidence of a filling defect (Figure 2).
Figure 1: White arrow indicating the urothelial tumour of the left renal pelvis. White circle indicating a non-fuctioning hydronephrotic kidney
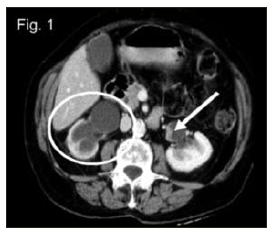
Figure 2: Nephrostogram showing contrast in the upper renal tract which does not extend below the angioplasty balloon (white arrow) in the mid left ureter.
Discussion
The incidence of upper urinary TCC following radical cystectomy for bladder urothelial cancer ranges from 2% to 6% with the majority of recurrences occurring within 3 years1. The standard treatment for upper tract TCC is radical nephroureterectomy, however, endoscopic percutaneous resection has become viable less invasive treatment option2 for those who would be rendered dialysis dependent following nephroureterectomy3. Resection modality may depend on tumour size and type and may involve cautery, laser, or electrovaporisation techniques2. Complications include bleeding, perforation of the renal pelvis and tumour seeding along the nephrostomy tract4. Repeat nephroscopy after 3 months has been recommended with radiological follow up at 6 month intervals5.
Antegrade renal pelvis instillation of BCG post endoscopic percutaneous resection has been shown to be well tolerated5 with reported lower recurrence rates in the patients with grade 1 TCC tumours, while no benefit was seen in those with grade 2 or 3 disease6. The largest series compared those treated with BCG post resection of upper tract TCC to those treated with resection alone showed no overall oncologic benefit between groups7 but did suggest a role for BCG in the management of upper tract CIS or intermediate or high grade disease in an anatomically or functionally solitary kidney8. Overall recurrence rates in patients receiving adjuvant BCG are approximately 33%8. Complications of upper tract BCG administration are uncommon and include BCG dissemination and urosepsis7. Percutaneous ureteric occlusion has been used in the management of fistulas of the lower urinary tract to allow diversion of urine using a variety of techniques including angioplasty balloons and has been shown to be well tolerated9. To our knowledge this is the first reported use of an inflated angioplasty balloon in the ureter to help localise BCG following antegrade renal pelvis instillation.
Correspondence: JC Forde
Department of Urology, St James’s Hospital, James’s St, Dublin 8
Email: [email protected]
References
1. Tran W, Serio AM, Raj GV, Dalbagni G, Vickers AJ, Bochner BH, Herr H, Donat SM. Longitudinal risk of upper tract recurrence following radical cystectomy for urothelial cancer and the potential implications for long-term surveillance. J Urol. 2008 Jan;179:96-100.
2. Tomaszewski JJ, Smaldone MC, Ost MC. Endourologic management of upper tract transitional cell carcinoma following cystectomy and urinary diversion. Adv Urol, 2009: 1-6.
3. Palou J, Piovesan LF, Huguet J, Salvador J, Vicente J, Villavicencio H. Percutaneous nephroscopic management of upper urinary tract transitional cell carcinoma: recurrence and long-term followup. J Urol. 2004 Jul;172:66-9.
4. Huang A, Low RK, deVere White R. Nephrostomy tract tumor seeding following percutaneous manipulation of a ureteral carcinoma. J Urol. 1995 Mar;153:1041-2.
5. Vasavada SP, Streem SB, Novick AC. Definitive tumor resection and percutaneous bacille Calmette-Guerin for management of renal pelvic transitional cell carcinoma in solitary kidneys. Urology. 1995 Mar;45:381-6.
6. Jabbour ME, Smith AD. Primary percutaneous approach to upper urinary tract transitional cell carcinoma. Urol Clin North Am. 2000 Nov;27:739-50.
7. Rastinehad AR, Ost MC, Vanderbrink BA, Greenberg KL, El-Hakim A, Marcovich R, Badlani GH, Smith AD. A 20-year experience with percutaneous resection of upper tract transitional carcinoma: is there an oncologic benefit with adjuvant Bacillus Calmette Guerin therapy? Urology. 2009 Jan;73:27-31.
8. Rastinehad AR, Smith AD. Bacillus Calmette-Guerin for upper tract urothelial cancer: is there a role? J Endourol. 2009 Apr;23:563-8.
9. Horenblas S, Kröger R, van Boven E, Meinhardt W, Newling DW. Use of balloon catheters for ureteral occlusion in urinary leakage. Eur Urol. 2000 Nov;38:613-7.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|