E Kilbride1, J Hussey2, G Boran1, P Greally1
1AMNCH, Tallaght, Dublin 24
2Department of Physiotherapy, School of Medicine, Trinity College Dublin
Abstract
Although the clinical signs of cardiovascular disease (CVD) are not evident until adulthood, many of the risk factors have their roots in early childhood. The aim of this study was to examine physical activity levels (PA) and the incidence of CVD risk factors in a small population (n=102) of primary school children in Dublin. Risk factors measured included overweight/obesity, blood lipids, blood pressure (BP), physical fitness and PA levels. Over a quarter of the group were overweight/obese (n=29, 28%). Despite relatively good fitness levels, PA levels were low with less than half the group (n=44, 46%) participating in the recommended 1hour/day. Fewer girls reported spending >1hour/day at PA compared to boys (n=14 v n=30). Six children had elevated cholesterol levels and five children had higher than normal BP values. Sixteen children demonstrated clustering of CVD risk factors and in those who were inactive the risk was greater. Our data suggest that in children as young as 10years significant risk factors already exist. Furthermore, the low level of PA in girls provides a target for health promotion programmes.
Introduction
It is widely accepted that many of the risk factors for cardiovascular disease (CVD) have their roots in early childhood and persist into adulthood. While there is a genetic component to the disease process, lifestyle also plays an important role. Physical inactivity, poor physical fitness, fat intake, blood pressure (BP) and an adverse lipid profile are all risk factors. Examining the relationship between these lifestyle parameters and CVD risk factors in children is vital to determine if lifestyle modifications during childhood and adolescence could lower CVD risk. Currently there is a lack of national reference values for children for these important health indicators. The aim of this study was to examine the incidence of CVD risk factors in children, and any relationship there may be between these risk factors and physical activity (PA) levels. Our results will provide an indication of the health status of children today. By identifying those at risk, appropriate lifestyle modifications can be made in an attempt to reduce their risk of developing CVD in later life.
Methods
Healthy school children from randomly selected primary schools volunteered to participate in the study between summers 2005-2007. Written informed consent was obtained from both the child and a parent/guardian and each child underwent a medical examination prior to participation. Height and weight were measured using a wall-mounted stadiometer and electronic scales. Lean body mass was measured by bioelectrical impedance analysis using a Tanita lean body mass scales (Model TBF-538). Information on dietary intake was not included in this study. Pubertal assessment was performed according to Tanner to ensure all children were pre-pubertal.1 Blood pressure was measured using a Spacelabs Medical BP monitor. Subjects provided a fasting blood sample to measure total cholesterol (TC), high-density lipoprotein (HDL-c), low-density lipoprotein (LDL-c), triglycerides (TG), C- reactive protein (CRP) and HbA1c. Physical activity (PA) was subjectively measured using a Modifiable Activity Questionnaire.2 Physical fitness (VO2max) was determined from an exercise test to exhaustion on a cycle ergometer (Ergoline, Germany). Heart rate and oxygen saturation were measured using a 3-lead ECG and pulse oximeter (Nonin 8600). Approval for the study was obtained from the Research Ethics Committee of SJH/AMNCH.
Results
102 children (50 boys) aged 10-12years participated in the study. Demographics are shown in table 1. Using age- and gender-specific BMI cut-off values proposed by the International Obesity Task Force,3 16% of boys were considered overweight and a further 6% obese, while values for girls were 31% and 4% respectively. The incidence of overweight or obesity for the group as a whole was 28% (boys 22%, girls 35%).
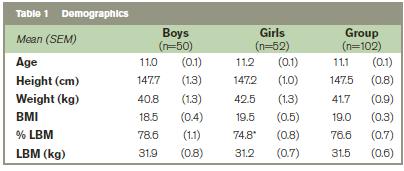
Mean (SEM) age, height, weight, BMI, body mass index, %LBM, percentage lean body mass and kilograms lean body mass. * p<0.01.
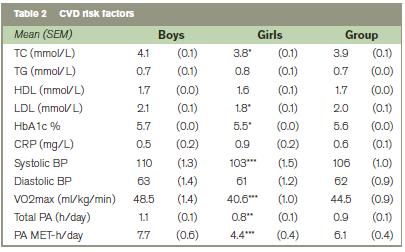
Mean (SEM) TC, total cholesterol, TG, triglycerides, HDL, high density lipoprotein, LDL, low density lipoprotein, HbA1c, CRP, C-reactive protein, systolic BP, diastolic BP, VO2max, maximum oxygen consumption, Total PA, total hours per day physical activity and MET-h/day, metabolic equivalent for physical activity. * p<0.05, ** p<0.01, *** p<0.001.
Table 2 shows blood lipid profiles, BP, physical fitness and PA for the two groups. High blood lipid concentrations were defined according to the American Academy of Paediatrics.4 Six children (3 boys) had total cholesterol (TC) and triglyceride (TG) levels above the recommended cut off points (>5.2mmol/L and >1.3mmol/L). C-reactive protein (CRP) values ranged from 0.1 to 5.9mg/L and values correlated significantly with BMI (0.36, p<0.01), VO2max (-0.43, p<0.001), PA (-0.28, p<0.05) and number of CVD risk factors (0.37, p<0.005). Four children (2 boys) had CRP values greater than 3mg/L, which the American Heart Association considers the cut off value for higher CVD risk in adults.5 Mean BP for both groups was within the normal range.6 Five boys had higher than normal BP values. Mean PA for the group was 0.9h/day, however, only 46% of the group actually participated in the recommended 1hour of PA per day, and this value was considerably lower in girls compared to boys (28% v 63%).
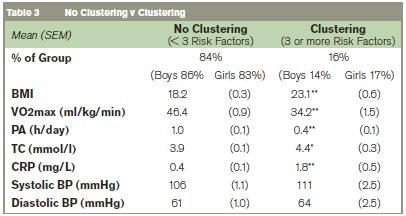
Mean (SEM) percentage of group, BMI, body mass index, VO2max, maximum oxygen consumption, PA, physical activity, TC, total cholesterol, CRP, C-reactive protein, systolic and diastolic blood pressure. *p<0.05, ** p<0.001.
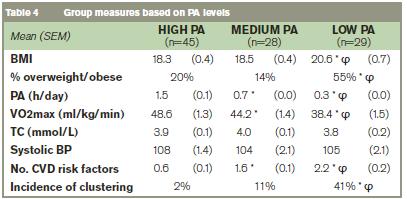
Mean (SEM) body mass index, percentage of children overweight or obese, PA, physical activity, VO2max, TC, total cholesterol, systolic BP, number of CVD risk factors and incidence of clustering for the three groups based on levels of PA. High = >60mins/day, Medium = 30-60mins/day, Low = <30mins/day. * Indicates significant difference from high group, ? indicates significant difference from medium group.
Clustering of CVD risk factors was described as having three or more of the following risk factors: overweight/obese, elevated TC, elevated BP, decreased PA (<1h/day) and decreased VO2max (below the mean for gender). 28% of children had no risk factors, 32% had one risk factor, 24% had 2 risk factors and 16% had 3 or more risk factors. Comparison of individual risk factors between children demonstrating clustering and those who did not are shown in table 3. To examine the effect of PA levels on clustering of CVD risk factors, we split the group into high (>60mins/day), medium (30-60mins/day) and low (<30mins/day) levels of PA. Results are shown in table 4.
Discussion
We aimed to examine PA levels and the incidence of CVD risk factors in a small group of primary school children in Dublin, Ireland. Risk factors measured included overweight/obesity, blood lipids, BP, physical fitness and PA levels. The health benefits of a physically active lifestyle in adults are well documented. In children associations have been shown between regular PA and reduced overweight/obesity and biological CVD risk factors.7,8 Obtaining accurate measures of PA is especially difficult in children. We used the modifiable activity questionnaire, which has been validated in adolescents2, as a subjective measure of PA. As children in this study were slightly younger, we administered the questionnaire jointly to the parent and child in an effort to record more reliable information. While questionnaires fail to capture spontaneous, unplanned activity, they provide the only feasible means of assessing PA in a large cohort. Current guidelines recommend that children participate in 1hour/day PA. While it appears our group complies with this, on closer inspection only 46% of the group actually participated in the recommended 1hour/day and this value was considerably lower in girls (28% v 63% boys). Comparing results between studies is difficult, due to the different methods used to measure PA. Results from the HSBC International report from 2005/2006 involving 41 countries, reported 30% of boys and 22% of girls participating in 1hour/day of moderate/vigorous PA.9 The group mean for Ireland was 45% (51% boys, 38% girls) which was the second highest overall and almost identical to our results. The importance of promoting PA in children remains clear, with particular emphasis on young girls where participation rates are low.
According to the National Task Force on Obesity, excess body weight is now the most prevalent childhood disease in Europe, affecting one in six children. 28% of our study group were overweight or obese, with a higher incidence in girls compared to boys (35% v 22%). These results are similar to previous studies from Ireland, the UK and the rest of Europe.10-12 Overweight/obesity rates for the US are reported to be slightly higher at approximately 31%, however this is based on the Centres for Disease Control and Prevention guidelines of a BMI greater than the 85th percentile for age.13 High TC levels in childhood play a role in the development of adult CVD, therefore reducing TC early in life would be beneficial in reducing future risk. TC in our group was within the normal healthy range (3.9mmol/L). These values are similar, if not more favourable, to previous studies from Northern Ireland and Europe.7,14,15
Based on the American Academy of Pediatrics’ recommendations, 6% of our group had TC levels above the recommended cut off point and half of these children were considered overweight or obese.
Mean BP for our group was within the normal range for age, height and gender and values were similar to previous reports of BP in children of this age.16,17 10% of boys showed abnormal BP values. Over half of these boys were overweight and the mean BMI was considerably higher than the rest of the group (20.9 v 18.3). These findings are in agreement with other studies reporting higher BP in children with higher BMI.18,19 High aerobic fitness during childhood and adolescence has been associated with a healthier cardiovascular profile not only during these years but also later in life.15 Our study group showed VO2max values similar, if not slightly higher, than those recently reported for European age-related peers.20,21 Direct measures of VO2max have not previously been reported in Irish children. Studies addressing fitness levels have used field-based tests as estimates of aerobic fitness. Therefore it is difficult to assess if fitness levels in Ireland have changed over the last 10-20years.
CRP is thought to be associated with the development of CVD in adults. Studies have also demonstrated that childhood CRP values predict adult CRP values.22 According to the American Heart Association, in adults CRP values <1mg/L indicate low risk of developing CVD, values between 1-3mg/L indicate average risk and values >3mg/L indicate high risk.5 In keeping with this we found a significant positive correlation between CRP and number of CVD risk factors (r=0.37, p<0.005). Several of these risk factors are often present in the same individual and this clustering is associated with an increased risk of CVD. Clustering of risk factors is therefore thought to be a better measure of cardiovascular health in young people than single risk factors alone. In this study we defined clustering as having three or more of the following risk factors: overweight/obesity, elevated TC, elevated BP, decreased physical fitness and decreased PA. We found evidence of clustering in 16% of our group. These children had significantly higher mean BMI and TC and significantly lower mean VO2max and PA levels compared to the rest of the group. A recent study involving European children have reported similar results with 15% of 9year olds showing clustering of CVD risk factors.23 CRP values were also significantly higher in the group demonstrating clustering, which adds support to the hypothesis that CRP plays a role in the pathogenesis of early atherosclerosis.
When we examined clustering with respect to PA, we found significantly lower PA levels in those who demonstrated clustering compared to those who did not (0.4h/day v 1.0h/day, p<0.001). Indeed 94% of children who had clustering of CVD risk factors had lower than recommended PA levels. Furthermore, of the children who did participated in the recommended 1h/day of PA only 2% showed clustering of risk factors. We further examined this relationship by splitting the group based on time spent at PA. The LOW group reported <30mins PA per day, the MEDIUM group 30-60mins PA per day and the HIGH group >60mins PA per day. The number of CVD risk factors was significantly greater in those who exercised for <60mins/day and significantly greater again for those exercising for <30mins/day. The incidence of clustering was also considerably higher in those who exercised for <30mins/day. A recent study in Sweden involving children of a similar age, also reported that those with low levels of PA have higher composite risk factor score for CVD.24 Our findings are consistent with the literature to date7,25 and highlight the importance of PA in childhood.
In conclusion, we have shown that in children as young as 10years significant CVD risk factors exist. Furthermore, one in six children showed evidence of clustering of these risk factors. Of particular note was the greater risk of clustering in children exercising for less than 30mins per day. As CVD risk factors are known to track into adulthood, our data provides support for preventative programs aimed at children, in particular targeting young girls where participation in regular physical activity is low.
Correspondence: E Kilbride
Children's Respiratory Lab, The National Children's Hospital, Tallaght, Dublin 24
Email: [email protected]
Acknowledgements
Dr Vincent Maher, Consultant Cardiologist, AMNCH, for his assistance in the planning of this study. Many thanks to The Ray D’Arcy show and Today FM who helped fund this study.
References
1. Tanner JM. Growth at Adolescence. Oxford UK, Blackwell Scientific Publications, 1962.
2. Aaron DJ, Kriska AM, Dearwater SR, Cauley JA, Metz KF and LaPorte RE. Reproducibility and validity of an epidemiologic questionnaire to assess past year physical activity in adolescents. Am J Epidemiol 1995;142:191-201.
3. Cole TJ, Bellizzi MC, Flegal K, and Dietz WH. Establishing a standard definition for childhood overweight and obesity worldwide: international survey. BMJ 2000;320:1240-1245.
4. Daniels SR and Greer FR. Lipid screening and cardiovascular health in childhood. Pediatrics 2008;122:198-208.
5. Pearson TA, Mensah GA, Alexander WR, Anderson JL, Cannon RO, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, Rifai N, Smith SC, Taubert K Tracy RP and 6. Vinicor F. Markers of Inflammation and Cardiovascular Disease. Circulation 2003;107:499-511.
6. National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents. Pediatrics 2004;114:555-576.
7. Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S and Anderssen SA. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study). Lancet 2006;368:299-304.
8. Kamtsios S and Digelidis N. Physical activity levels, exercise attitudes, self-perceptions and BMI type of 11 to 12-year-old children. J Child Health Care 2008;12:232-240.
9. HBSC International Report from 2005/2006: Inequalities in young people’s health. World Health Organisation 2008 Chapter 2.
10. Whelton H, Harrington J, Crowley E, Kelleher V, Cronin M and Perry IJ. Prevalence of overweight and obesity on the island of Ireland: results from the North South Survey of Children’s Height, Weight and Body Mass Index, 2002. BMC Public Health 2007;7:187-194.
11. Stamatakis E. Health Survey for England 2002: The health of children and young people. Stationary Office, London. [www.dh.gov.uk/en/Publicationsandstatistics/publications/publicationstatistics/DH_4078027] (accessed February 2010).
12. Lobstein T and Frelut ML. Prevalence of overweight among children in Europe. Obes Rev 2003;4:195-200.
13. Ogden L, Carroll MD and Flegal KM. High body mass index for age among US children and adolescents, 2003-2006. JAMA 2008;299(20):2401-2405.
14. Boreham C, Twisk J, Neville C, Savage M, Murray L and Gallagher A. Associations between physical fitness and activity patterns during adolescence and cardiovascular risk factors in young adulthood: The Northern Ireland Young Hearts Project. Int J Sports Med 2002;23:S22-S26.
15. Rizzo NS, Ruiz JR, Hurtig-Wennlof A, Ortega FB and Sjostrom M. Relationship of physical activity, fitness, and fatness with clustered metabolic risk in children and adolescents: The European Youth Heart Study. J Pediatr 2007;150:388-394.
16. Bouziotas C, Koutedakis Y, Nevill A, Ageli E, Tsigilis N, Nikolaou A and Nakou A. Greek adolescents, fitness, fatness, fat intake, activity and coronary heart disease risk. Arch Dis Child 2004;89:41-44.
17. Anderssen SA, Cooper AR, Riddoch C, Sardinha LB, Harro M, Brage S and Andersen LB. Low cardiorespiratory fitness is a strong predictor for clustering of cardiovascular disease risk factors in children independent of country, age and sex. Eur J Cardio Prev Rehab 2007;14:526-531.
18. Botton J, Heude B, Kettanah A, Borys JM, Lommex A, Bresson JL, Ducimetiere P and Charles MA. Cardiovascular risk factor levels and their relationships with overweight and fat distribution in children: the Fleurbaix Laventie Ville Sante II study. Metabolism 2007;56:614-622.
19. Barath A, Boda K, Tichy M, Karoly E and Turi S. International comparison of blood pressure and BMI values in schoolchildren aged 11-16years. Acta Paediatrica 2009
20. Ruiz JR, Ortega FB, Rizzo NS, Villa I, Hurtig-Wennlöf A, Oja L and Sjöström M. High cardiovascular fitness is associated with low metabolic risk score in children: The European Youth Heart Study. Pediatr Res. 2007;61:350-355.
21. Steene-Johannessen J, Kolle E, Anderessen SA and Andersen LB. Cardiovascular disease risk factors in a population-based sample of Norwegian children and adolescents. The Scand J Clin Lab Invest. 2009;69:380-386.
22. Juonala M, Viikari J, Rönnemaa T, Leena T, Marniemi J and Raitakari OT. Childhood C-reactive Protein in Predicting CRP and Carotid Intima-Media Thickening in Adulthood. The Cardiovascular Risk in Young Finns Study. Arterioscler Thromb Vasc Biol. 2006;26:1883-1888.
23. Froberg K and Andersen LB. Mini Review: Physical activity and fitness and its relations to cardiovascular disease risk factors in children. Int J Obes (Lond) 2005;29:S34-S39.
24. Tanha T, Wollmer P, Thorsson O, Karlsson MK, Linden C, Andersen LB and Denker M. Lack of physical activity in young children is related to higher composite risk factor score for cardiovascular disease. Acta Paediatrica 2011;100:717-721.
25. Ribeiro JC, Guerra S, Oliveira J, Teixeira-Pinto A, Twisk JW, Duarte JA and Mota J. Physical activity and biological risk factors clustering in paediatric population. Prev Med 2004;39:596-601.