|
|
|
|
|
|
|
|
Ciaran Somers,O'Connor J
|
|
|
Ir Med J. 2012 Oct;105(9):295-8
CJ Somers, J O'Connor
The Drug Treatment Centre Board, McCarthy Centre, 30-31 Pearse St, Dublin 2
Abstract
Retrospective study of urinary heroin outcomes of a cohort (123) of patients commenced on a methadone treatment program. Significantly poorer outcomes were associated with urines positive for cocaine (OR 0.69 CI 0.59-0.81) benzodiazepines (OR 0.7 CI 0.53-0.93) with prescribing of low dose methadone (OR 0.65 CI 0.48-0.87), with urines positive for heroin at time of admission (OR 0.74 CI 0.56-0.97) and with behavioural sanctions (OR 0.8, CI 0.65-0.98). Improved outcomes were associated with granting of take away methadone (OR 1.34 CI 1.1-1.62). with an indication of improved outcomes associated with alcohol positive urines (OR 1.34 CI 0.95-1.9) and increased duration of clinic attendance (OR 1.21 CI 0.99-1.47). On multiple regression analysis low dose methadone (0.07 CI 0.01-0.33) prescribing remained negatively associated with urine heroin outcomes.
|
|
Introduction
A meta analysis by Matick et al1 showed that oral methadone was an effective opiate maintenance therapy retaining patients in treatment and decreasing heroin use. Contemporaneous studies described methadone doses of 60 mg and greater giving better outcomes compared to lower doses2,3. The effectivness of established methadone treatment programs for substance abusers was supported by outcome studies including DATOS4(USA), NTORS5 (England and Wales), the ROSIE6 study providing the first longitudinal data for methadone treatment in Ireland, This showed a sustained reduction in the use of a number of substances over a 3 year period. Methadone has been described as protective against combined heroin and cocaine use7 but adverse effects of benzodiazepine use by clients prescribed methadone were reported8. In a DTCB based study Kamal et al9 concluded that use of cocaine and benzodiazepines caused poorer outcomes for methadone subjects. Methadone subjects abstaining from alcohol were reported as less likely to use other substances10 and Byrne and Petry11 described alcohol dependent patients taking methadone having a longer duration of cocaine abstinence than non alcohol dependent. Increased prevalence of cannabis use by those prescribed methadone (6.2% - 39%), as compared to the normal US population (5.8%) was reported by Reisfield et al12.
The Present study is retrospective and designed to look at treatment outcomes for a cohort of clients attending a methadone clinic. The primary outcome was defined as subjects with all urine samples negative for heroin or with less than 20 % of samples positive for heroin. The objective was to analyse the effect of factors including co morbid substance use, methadone dose and behavioural and socio demographic on this outcome and comparing it with an earlier DTCB (Drug Treatment Centre Board) based study9. The derived information should lead to an improvement in the management of substance abusing subjects both in Ireland and internationally
Methods
The design is a retrospective cohort study of outcomes of all clients admitted to a DTCB sector for treatment with methadone during 2008. Where clients were admitted more than once during this period, only the first admission was included. Excluded were clients who discontinued attending the clinic during the initial 3 month period, clients who were retro viruse positive and those who became pregnant. The effect of different parameters including socio demographic, psychiatric diagnosis, use of other illicit substances, client behaviours and prescription of antibiotics specific for soft tissue infections were examined using univariate and multivariate analyses.
Prescribed methadone dose and urine analyses for heroin, cocaine, benzodiazepines, alcohol, cannabis and amphetamines, were recorded at 3, 9 and 15 months post admission and also at the time of admission to provide a base line for the subjects. Occurrrence of the following variables was determined between the end of the 3rd and 15th months: periods of low dose (20 mg) methadone prescribing; clients sanctioned for mis behaviour; take aways awarded for consistent provision of substance negative urines; courses of flucloxacillin prescribed (indicator of soft tissue infection treatment)13. Socio demographic data recorded included age, sex, accommodation status, number of admissions to the clinic and dual diagnosis. Dual diagnosis was recorded from the clinical notes and did not involve use of a structured diagnostic instrument. Where a co morbid psychiatric diagnosis was not recorded in the clinical notes it was assumed for the purposes of the study that none was present. Urine samples were screened for the different substances at the DTCB laboratory to ISO/IEC 17025 standard by routine immunoassay14.
Associations between categorical variables and outcomes were examined using Pearsons Chi squared test. Odds ratios and their 95% confidence intervals were reported to indicate the magnitude of associations. Separate univariate analyses were carried out for 3, 9 and 15 month time intervals and for the combined data. Socio demographic parameters, methadone dose and urine analyses for clients entering the study and those excluded were compared using either mean values or frequencies. A logistic regression analysis, including all variables which gave a significance value less than 0.1 on univariate analysis, was done to identify those variables independently predictive of urine heroin outcome. Data was analysed using SPSS version 18. The study was approved by the DTCB Ethics Committee.
Results
25.5 % from the total 165 admissions during the period of the study (2008) were of one or more repeat admissions of clients. Of the remaining 123 first admissions, 4 were excluded because of retro viral therapy and 2 because of pregnancy. Table 1 includes methadone dose, urine substance analyses and demographic parameters and compares those clients included in the study (80) and those who stopped attending before the end of third month (excluded) (37). Repeat admissions were significanty greater for those who had stopped attending at 3 months. 52.5% of the subjects were prescribed 1 or more methadone take away doses, 63.3% low dose methadone, 15% were sanctioned for a behaviour and 18.2% were prescribed flucloxacillin.
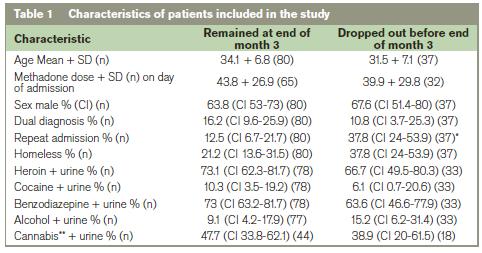
*Significant difference at 5% level.
** Numbers of urines anaysed for cannabis were less due to clinical policy.
SD = Standard deviation
CI = Confidence interval
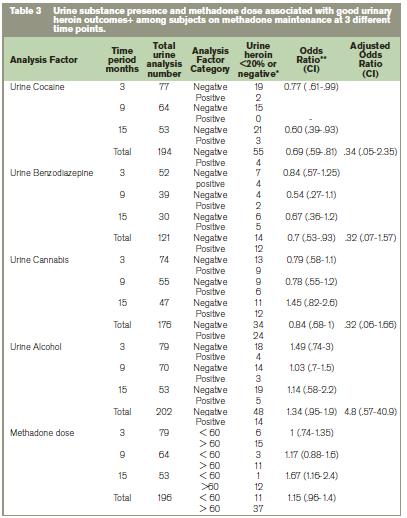
Table 2 shows prescribed methadone doses and urine analyses for the subjects at 3 time points. Of the 80 subjects attending at 3 months, 66 remained at 9 and 56 at 15 months. The other subjects had stopped attending. Only a third of urine samples or less were analysed for alcohol, cannabis and amphetamines compared to other substances, according to the clinical practice at DTCB. As a result it was not possible to present an intermittent positive category for the cannabis results. Significant differences were present between times for urine cocaine analysis only (p<0.05). Number of regular cocaine positive urines increased with duration of attendance. Urines were amphetamine positive for 2 subjects only (2.5%).Table 3 shows the relationship between urine heroin outcome and presence of other substances and methadone dose for the 3 time intervals and the pooled value as the odds ratios. Significantly poorer outcomes were associated with urines positive for cocaine (OR 0.69 CI 0.59-0.81) and benzodiazepines (OR 0.7 CI 0.53-0.93). Methadone dose at 15 months was associated with an improved outcome (OR 0.1.67 CI 1.16-2.41), with an indication of an improved outcome associated with alcohol positive urines (OR 1.34 CI 0.95-1.9).
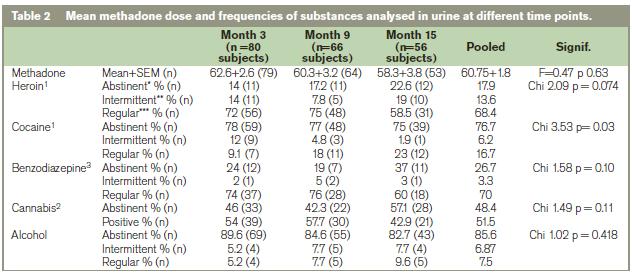
*Abstinent = urines negative for substance (n)
** Intermittent = less than 20% of urines substance positive (n)
*** Regular = greater than 20 % of urines substance positive (n)
1Analyses were determined at random once or twice weekly during the 8 week period following the individual time points
(% value is for 5-8 urine samples per subject for heroin, cocaine and benzodiazepines and 2-3 samples for alcohol and cannabis)
2An intermittent positive category could not be determined in the case of cannabis as there were insufficient urine samples.
3Adjusted for prescribed benzodiazepines
Table 4 shows the relationship between urine heroin outcomes and behavioural and urine substance analysis at time of admission. Improved outcomes were associated with granting of take away methadone (OR 1.34 CI 1.1-1.6) with increased duration of clinic attendance bordering on significance (OR of 1.2 CI 0.99-1.5). Poorer outcomes were associated with heroin positive urine at day of admission (OR 0.74 CI 0.56-0.97), prescribing of low dose methadone (OR 0.65 CI 0.48-0.87) and behavioural sanctions (OR 0.8, CI 0.65-0.98 ). On multiple regression analysis low dose methadone (0.07 CI 0.01-0.33) prescribing was negatively associated with urine heroin outcome (see table 4). At end of 3rd month, for those on a methadone dose of less 60 mg, 13.6% (4) were heroin abstinent in urine. Of the 3 clients prescribed more than 100 mg of methadone, none were abstinent and 2 had more than 20% urine specimens positive for heroin.
+ A good outcome is defined as negative or less than 20% of urine specimens testing positive for heroin during an 8 week period post the stated time point 14.
*Only abstinent and intermittently heroin positive urines were included in this outcome analysis as these results met the criteria for good outcomes.
** An odds ratio greater than 1 corresponds to a positive effect on urinary heroin outcome and less than 1 to a negative effect on this outcome.
CI = Confidence Interval
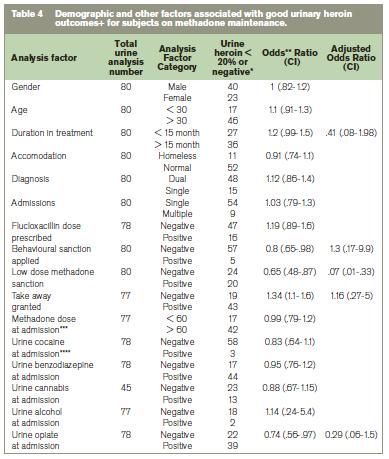
+ A good outcome is defined as less than 20% of urine specimens testing positive for heroin during 8 week period post stated time point14.
*Only abstinent and intermittently heroin positive urines were included in this outcome analysis as these results met the criteria for good outcomes.
** An odds ratio greater than 1 corresponds to an improved urinary heroin outcome and less than 1 to a disimproved outcome.
*** Refers to most recent methadone dose prescribed during the 2 week period preceding admission.
**** Refers to analysis result for routine urine taken on the day of admission to the program.
CI = Confidence Interval
Discussion
The percentage of heroin positive urines reported for our subjects (pooled value of 82%) is greater than value of 66% reported for DTCB subjects in 20049. The overall mean daily methadone dose prescribed for the present study was 60.75+25 mg compared to 74 mg in the earlier study. A methadone dose above 60 mg led to an significantly improved outcome in present study at 15 months. Improved outcomes and greater retention in treatment at higher methadone doses are widely reported9,15,3. The incidence of cocaine positive urines for our subjects at 22.9%, for pooled time intervals, is lower compared to 39% reported by Kamal et al9. Thula16 reported that 9% of clients attending DTCB, had greater than 50 % of their urines positive for cocaine. The direct comparative figure was 6.6% cocaine positive urines for present study. The urine analyses tentatively indicate that there has been a decline in the incidence of cocaine positive urines at DTCB since 2004. Such reduction a cocaine use may reflect differences in availability of supply of the substance between the 2 periods. The NACD17 reported a life time prevalence for cocaine use in the general population in Ireland as 8% (age 15-34) and 3% (age 35-64). Reported figures for cocaine use by those on methadone treatment for other locations range from 14% to 55 %18,19.
Urine benzodiazepine (73.3%) and alcohol (14%) presence for combined data was similar to previous DTCB figures9. The comparison is for subjects not prescribed benzodiazepines. Published studies for benzodiazepine use by clients on methadone include values above 50%20. In the present study there was an indication that alcohol use increased with time attending the clinic. Ryder et al21 in an Irish general practice survey of methadone clients found that 14% met criteria for alcohol dependence using the AUDIT screening test. Our results for cannabis positive urines (51.5%) compare to published values 54%22 for subjects on methadone treatment.
The present finding of poorer outcomes for methadone treated clients who used cocaine and non prescribed benzodiazepiness are consistent with Karmal et al9. Poor outcomes associated with cocaine use are reported by a number of authors23,3 and associated with benzodiazepine use by others9,20. The poorer outcomes for clients prescribed low dose methadone (20 mg) agree with published findings24 that such a dose is sub therapeutic. There was an indication from our findings of improved urine heroin outcomes for clients using alcohol. Kamal et al9 findings indicated improved urine heroin outcomes for regular alcohol users but the results were non significant A reduction in heroin positive urines for clients taking alcohol might tentatively be related to these clients having a reduced requirement for heroin. The significantly improved outcomes for clients prescribed take away methadone confirms that the granting of take aways is dependent on the provision of clean urines by the attending clients. The positive association between behavioural sanctions and poorer urinary heroin outcomes provides further evidence that adverse client behaviour is related to heroin use for patients prescribed methadone.
Limitations of this study include the exclusion of subjects who dropped out before 3 months. They had significantly more repeat admissions compared to those remaining. Numbers were small, including only subjects from one DTCB sector9. DTCB, which is a specialised methadone clinic, has clients with more chronic substance abuse problems and may not be a truly representative population9. The primary outcome of this study was the presence of heroin in urine. As previously described9 urine analysis is an objective method for detecting illicit substance use, but is confounded by differences in elimination half life. Co morbid psychiatric illness as reported here was based on diagnosis in the clinical notes and not derived using a structured diagnostic instrument. The clinical notes did not always record whether or not a dual diagnosis was present and it was assumed for the purposes of the study that these clients did not have a dual diagnosis. Our values for presence of a dual diagnosis may as a result be an under estimate. A randomised control double blind study would have been a more appropriate statistical design for this this study with allocation of clients to specific methadone doses.
Benefits of this study are that it can be compared with previous studies carried out at the same centre since 20049,16 It provides data on the same patient sample at 3 time intervals and on behavioural outcomes, antibiotic prescribing and provides information on cannabis use which was absent from an earlier study9. In conclusion cocaine and benzodiazepine abuse by clients and prescribing of low dose methadone were significant factors negatively impacting on methadone outcomes. A prospective study should be undertaken of all clients attending DTCB service looking at the effects of variable methadone doses, of subject councelling and co morbid psychiatric illness on heroin use and client behavioural outcomes.
Correspondence: CJ Somers
St Vincent's Hospital, Richmond Road, Fairview, Dublin 3
Email: [email protected]
Acknowledgements
The contribution of nursing, laboratory and other staff at DTCB to this study. R Conroy, RCSI for valuable comments on the statistical methodology.
References
1. Mattick RP, Breen C, Kimber J and Davoli M. (2009). Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst. Rev. 8.
2. Fareed A, Casarella J, Roberts M, Sleboda M, Amar R, Vayalapalli S, and Drexler, K (2009). High dose versus moderate dose methadone maintenance: is there a better outcome? J. Addict. Dis. 28: 399-405.
3. Salamina G, Diecidue R, Vigna-Taglianti F, Jarre P, Schifano P, Bargagli AM, Davoli M, Amato L, Perucci CA, and Faggiano F (2010). Effectiveness of therapies for heroin addiction in retaining patients in treatment: results from the VEdeTTE study. Subst. Use Misuse. 45: 2076-92.
4. Hubbard, R.L, Craddock, J. and Anderson J. (2003). Overview of 5-year follow up outcomes in the drug abuse treatment outcome studies (DATOS). J. Subst. Abuse Treat. 25: 125-34.
5. Gossop M, Marsden J, Stewart D, and Treacy S. (2002). Change and stability of change after treatment of drug misuse: 2-year outcomes from the National Treatment Outcome Research Study (UK). Addict Behav. 27: 155-66.
6. Comiskey C.M , Kelly P, Leckey Y, McCulloch, L, O’Duill, B, R. Stapleton S. G, and White E. (2009). ROSIE Study. (Research Outcome Study in Ireland Evaluating Drug Treatment Effectiveness). Dublin: National Advisory Committee on Drugs.
7. Bravo MJ, Llorens N, Barrio G, Brugal MT, Santos S, Sordo L, and de la Fuente L. (2010). Methadone maintenance treatment: a protective factor for cocaine injection in a street-recruited cohort of heroin users. Drug Alcohol Depend. 1. 12: 62-8.
8. Brands B, Blake J, Marsh DC, Sproule B, Jeyapalan R, and Li S. (2008). The impact of benzodiazepine use on methadone maintenance treatment outcomes. J. Addict. Dis. 27: 37-48.
9. Kamal F, Flavin S, Campbell F, Behan C, Fagan J, and Smyth R. (2007). Factors affecting the outcome of methadone maintenance treatment in opiate dependence. Ir Med J. 100: 393-7.
10. Stapleton RD and Comiskey C M. (2010). Alcohol usage and associated treatment outcomes for opiate users entering treatment in Ireland. Drug Alcohol Depend. 1.107: 56-61.
11. Byrne SA and Petry N.M (2011). Concurrent alcohol dependence among methadone-maintained cocaine abusers is associated with greater abstinence. Exp. Clin. Psychopharmacol. 19: 116-22.
12. Reisfield GM, Wasan AD, and Jamison RN. (2009). The prevalence and significance of cannabis use in patients prescribed chronic opioid therapy: a review of the extant literature. Pain Med. 10: 1434-41.
13. The Sanford Guide to Antimicrobial Therapy ( 2000). 13 th. edition. D.N. Gilbert, R.C. Moellering, M.A. Sande. Antimicrobial Therapy. Inc. P.O. Box. 70, 229 Main st., Hyde Park, VT 05655, USA.
14. Pavlic, M. Libiseller, K., Grubwieser, P. and Rabl, W. (2005). Cross-reactivity of the CEDIA buprenorphine assay with opiates: an Austrian phenomenon. Int. J. Legal Med. 119: 378-81.
15. Peles E, Linzy S, Kreek M, and Adelson M. (2008). One-year and cumulative retention as predictors of success in methadone maintenance treatment: a comparison of two clinics in the United States and Israel. J. Addict. Dis. 27: 11-25.
16. Thula, M.A. (2009). Cocaine use and dependence in clients attending a drug treatment centre in Dublin. Psychiatric Bulletin 33: 88-91.
17. National Advisory Committee on Drugs. (2007). An overview of cocaine use in Ireland 11. Government Publications, Postal Trade Section, 51 St. Stephen's Green, Dublin 2.
18. Schottenfeld RS, Chawarski MC, Pakes JR, Pantalon MV, Carroll KM, and Kosten TR. (2005). Methadone versus buprenorphine with contingency management or performance feedback for cocaine and opioid dependence. Am J Psychiatry. 162: 340-9.
19. DeFulio A, and Silverman K. (2011). Employment-based abstinence reinforcement as a maintenance intervention for the treatment of cocaine dependence: post-intervention outcomes. Addiction. 106: 960-7.
20. Pattanayak RD, Jain R, and Ray R. (2011).Comparison of self-reported benzodiazepine use and urinalysis among consecutive treatment seekers at a tertiary care drug dependence treatment centre. Indian J. Physiol. Pharmacol. 54: 337-43.
21. Ryder N, Cullen W, Barry J, Bury G, Keenan E, and Smyth BP. (2009). Prevalence of problem alcohol use among patients attending primary care for methadone treatment. BMC Fam Pract. 11: 10, 42.
22. Kidorf M, Neufeld K, King VL, Clark M, and Brooner RK. (2007). A stepped care approach for reducing cannabis use in opioid-dependent outpatients. J Subst Abuse Treat. 32: 341-7.
23. Marsden J, Eastwood B, Bradbury C, Dale-Perera A, Farrell M, Hammond P, Knight J,Randhawa K, and Wright C. (2009). National Drug Treatment Monitoring System Outcomes Study Group Effectiveness of community treatments for heroin and crack cocaine addiction in England: a prospective, in-treatment cohort study. Lancet. 10. 374: 1262-70.
24. Donny EC, Walsh SL, Bigelow GE, Eissenberg T, Stitzer M L. (2002). High dose methadone produces superior opioid blockade and comparable withdrawal suppression to lower doses in opioid-dependent humans. Psychopharmacology (Berl). 161: 202-12.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|