|
|
|
|
|
|
|
|
AE Bennett,AL O'Connor,N Canning,A Kenny,EM Keaveney,KM Younger,MAT Flynn
|
|
|
Ir Med J. 2012 Sep;105(8):266-8
AE Bennett1, AL O'Connor1, N Canning1, A Kenny1, E Keaveney1, K Younger2, MAT Flynn1
1Food Safety Authority of Ireland, Abbey Court, Lower Abbey St, Dublin 1
2School of Biological Sciences, DIT, Kevin St, Dublin 8
|
|
Abstract
Weaning - the transition from milk to solid food - influences life-long health. Dietary challenges during weaning include providing sufficient critical nutrients such as iron with minimal added sugar and fat and no added salt. This study assessed the inclusion of iron-containing red meat in infant diets before age one year, and the Irish commercial baby food environment. Of mothers with an infant under 30 months of age who were surveyed in shopping centres in Ireland (n195), 82% (n159) reported wanting more weaning information. A quarter (n24) of infants over age 12 months (n97) received no iron-containing red meat before age one year. A scan of commercial baby foods in Ireland identified 448 products. While all complied with baby food legislation, 15% (n69) were intrinsically high in sugar and fat, or contained added salt. This study indicates the need for specific guidance on best infant feeding practice in Ireland.
Introduction
Weaning, defined as the transition from milk to solid food during the first year of life, is a process important for not only nutritional and developmental reasons1, but also for its potential influence on life-long feeding patterns and health1,2. It is currently recommended that the weaning process commence around six months of age3,4, when the volume of milk ingested by exclusively breastfed infants becomes insufficient to meet their nutritional requirements5. Studies suggest that flavour experiences and food preferences during infancy track into childhood and adolescence6. Since infants have an innate preference for sweet and salty tastes6, best practice in infant feeding5 advises non-bulky savoury and plain-tasting foods to help set the infant’s threshold for these tastes at lower levels later in life5. However, infants’ high nutritional requirements coupled with their capacity to consume relatively small amounts of food4 presents the challenge of providing sufficient nutrients with minimal added sugar and fat and no added salt4.
Recent Irish research has highlighted suboptimal feeding practices during this transition, to include weaning as early as six weeks of age7 and introducing foods at variance with best practice infant feeding guidelines, such as chocolates, biscuits, crisps and carbonated drinks7. Such weaning practices may increase the risk of childhood obesity2,8, the seriousness of which stems from its association with cardiovascular disease, type II diabetes mellitus, and cancer9. Ireland has high rates of childhood obesity, with a quarter of children aged four to sixteen years being overweight or obese10. Furthermore, children are not equipped to handle the prejudice and stereotyping associated with obesity11, resulting in adverse social and psychological functioning12. As such, this is a critical period for developing obesity, but equally an opportune time to intervene on, or preferably prevent, it.
The food environment must be considered when addressing the burden of obesity and associated chronic disease9,13,14. An infant’s food environment is determined by direct (micro-level) and indirect (macro-level) influences12. A highly influential micro-level influence is the home feeding environment, which is in turn affected by macro-level factors such as food availability, price, marketing, and societal issues9. The increasing burden of childhood obesity15 makes it essential that parents have the correct knowledge to make positive food choices on behalf of their children15, ideally within an environment that promotes optimal food choices14. The introduction of dietary sources of haem iron from six months of age to coincide with the depletion of iron stores from birth5 is an important infant feeding issue. Iron deficiency anaemia has been reported as an issue of concern amongst infants in Ireland16. Evidence suggests that even mild anaemia in infancy can adversely affect long-term mental and psychomotor development17,18.
The primary aim of this study was to examine the introduction of haem iron-containing foods, particularly red meat, into infant diets during the first year of life. The secondary aim was to assess the range of commercial infant foods available in Ireland.
Methods
The study sample was obtained in three urban and two rural shopping centres across Dublin and Laois. Census data19 were used to categorise each shopping centre location according to relative deprivation in Ireland. The resulting categories were: Disadvantaged Inner City Area, Affluent City Area, and Socioeconomically Mixed Rural District19. Women passing the survey stand who appeared to be of child-bearing age were invited to participate if they had an infant less than 30 months of age. A standardised, pilot-tested questionnaire obtained information on the age of the youngest child, mother’s age group, and age of first non-milk food. The inclusion of 9 common dietary sources of iron, including foods recommended for infants (beef, lamb, pork, chicken, oily fish, white fish) and foods not recommended for infants (ham, sausages, liver) was assessed. Mothers’ awareness of the age at which iron is important in the infant diet and their use of commercial infant foods were also assessed.
A scan of commercial infant foods marketed by infant food companies in supermarket multiples in Ireland was conducted. Information such as the product name, meal category, age grouping, presence of gluten, and available nutritional information per 100 grams of product was tabulated. Information was gathered from products on supermarket shelves, and website, telephone, and email services offered by manufacturers. All products were compared with European Union legislation 2006/125/EC to ensure compliance with essential composition. Commercial infant desserts and snacks which were not fruit- or dairy- based and commercial infant foods containing cured meats were listed as being at variance with best practice infant feeding guidelines, which advise minimal added sugar and fat and no added salt. SPSS Statistics version 18.0 was used. Statistical significance was p<0.05. Normally distributed categorical data were analysed using cross-tabulations and chi-squared statistical tests. Independent-samples t-tests assessed considerations mothers had on providing meat to an infant.
Results
Social and demographic characteristics
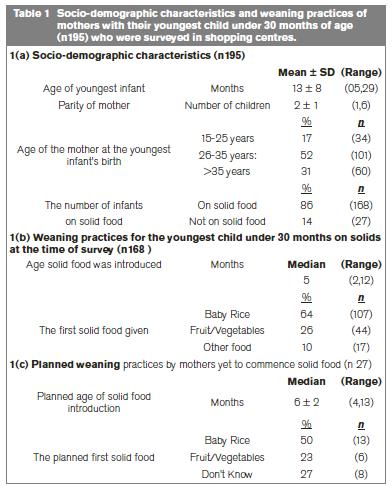
The demographic characteristics and weaning practices of study participants (n195) are presented in Table 1. Twenty-three per cent (n44), 36% (n71) and 41% (n80) of mothers were surveyed in the Disadvantaged Inner City Area, an Affluent City Area, and a Socioeconomically Mixed Rural District respectively. Most infants in this study (97%, n190) were born in Ireland. Two percent (n3) of infants were consuming a vegetarian diet. The public health nurse was regarded as the most useful source of infant feeding information, as reported by 29% (n57) of mothers. Of the total group, 82% (n159) of mothers felt that there should be more information available on weaning infants onto solid foods.
Introduction and consumption of iron-containing foods in the first year of life
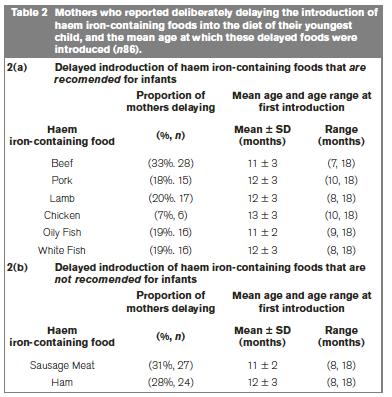
Of the 97 infants aged over 12 months, 68% (n66), 39% (n38), and 52% (n50) of infants received beef, pork and lamb respectively before 12 months. Half of these infants also received sausages (51%, n49) and ham (53%, n51) before 12 months of age. A quarter of infants (n24) received none of the recommended red meats (beef, lamb and pork) before 12 months of age. Mothers of infants under 12 months (n98) reported planning to introduce iron-containing foods at 8.1 ± 1.8 months. The majority of mothers (89%, n86) with infants over 12 months of age (n97) reported deliberately delaying feeding particular iron-containing foods to their infant during the first year of life (Table 2). Most mothers who delayed recommended red meats did so because they considered them to be inappropriate for infants (Beef: 75%, n21; Lamb: 77%, n13; Pork: 47%, n7). “Inappropriate foods” encompassed mothers’ concerns regarding the infant’s dentition, ability to swallow meat, and fragile digestive system.
Mothers’ knowledge influenced the introduction of iron-containing foods
Less than a third of mothers (31%, n60) from the whole group reported the correct age at which iron is important in infant diets. These mothers (n60) introduced recommended red meat significantly earlier (mean age of 7.1 ± 1.5 months) than mothers who were not aware of this age (n135; mean age 8.4 ± 2.5 months, p=0.006).
Mothers’ considerations regarding red meat introduction may impact the timing of red meat introduction
The most common considerations mothers had about introducing red meat into their infant's diet was the perceived 'risk of choking' (59%, n115) and the belief that meat 'texture is too tough' (47%, n92). The mean age of red meat introduction was significantly different (p=0.03) between mothers who reported that the tougher texture of meat was a consideration (8.4 ± 2.3 months, n70) and those who did not (7.5 ± 2.3 months, n54).
Scan of commercially available infant foods
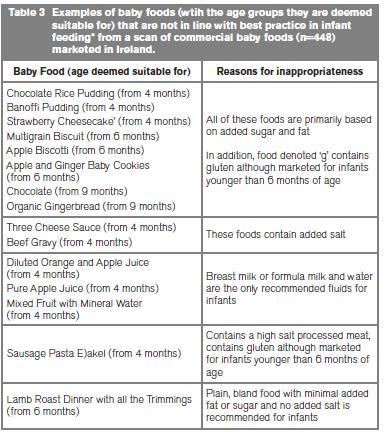
The scan of commercial infant foods identified 448 such foods available in Ireland. The nutritional composition provided on the label of each product complied with European Union Commission Directive 2006/125/EC. Some foods (15%, n69) did not emulate best practice infant feeding guidelines (Table 3), as they were intrinsically high in sugar, fat or contained added salt. Over two-thirds (68%, n113) of mothers surveyed used commercial baby foods, and 32% (n62) of mothers used the names of commercial infant foods as ideas for homemade meals.
Discussion
This study identified issues of concern relevant to infant feeding in Ireland. Most mothers surveyed wanted more information on weaning infants onto solid foods. A quarter of mothers did not introduce any recommended red meat in the first year of life and two-thirds of mothers did not know the age at which iron is important in the infant diet. The scan of commercial infant foods highlighted products at variance with best practice infant feeding. With respect to haem iron, the delayed provision, or absence altogether, of recommended red meat in infant diets increases the risk of iron deficiency and its associated adverse consequences17,18. The reported lack of knowledge about the importance of iron in the infant diet and the perceived inability of the infant to safely digest recommended red meats indicates the need for parental education on infant feeding. Mothers aware of the age at which iron is important in the infant diet introduced red meats significantly earlier than those who were not aware of this, further indicating the role of education. Such education should encompass the timely introduction of haem iron-containing foods and dispel unfounded concerns regarding infants' ability to consume red meat.
It is also important to recognise the role of non-haem iron food sources such as fortified cereals and follow-on formulas, especially in infant diets lacking haem iron food sources. Regular consumption of these foods can help to prevent iron deficiency. However, due to the lower bioavailability of non-haem iron, recommended red meats should be encouraged to provide not only highly bioavailable haem iron, but also greater variety and texture in the diet. A number of commercial infant foods did not emulate best practice infant feeding as they were intrinsically high in sugar, fat, or contained added salt. The potentially negative influence of these foods on infant feeding practices should be recognised, since a third of mothers reported using such foods as ideas for homemade recipes.
This study highlights areas of concern regarding infant feeding in Ireland; however, a number of study limitations must be acknowledged. It was not possible to ask all women of child-bearing age passing the stand to participate in the study due to a limited number of researchers. As such, sampling bias must be considered. Additionally, mothers’ socioeconomic status was categorised according to the location of the shopping centre in which they were surveyed. No other measures of socioeconomic status were assessed since requesting this sensitive information in a shopping environment was deemed inappropriate. Finally, this study is not nationally representative, and its design does not permit inference about causality from the results obtained.
Parental education on best practice in infant feeding is needed to promote suitable food choices on behalf of children. However, nutrition education in isolation has minor and short-lived effects at best20. Therefore, measures at the family level must be matched by changes in the larger environment, such as changes in industry and legislation, to help sustain positive health choices made by parents on behalf of their children21. A gap in parents’ knowledge on infant feeding has been identified in this study. The possible influence of commercial baby foods which are at variance with best infant feeding practice is a concern in terms of obesity and chronic disease. Therefore, whilst education is essential to inform parents, the commercial baby food industry equally has a role to play in creating a more supportive environment for best practice in infant feeding.
Correspondence: MAT Flynn
Food Safety Authority of Ireland, Abbey Court, Lower Abbey St, Dublin 1
Email: [email protected]
References
1. Barker DJP, Eriksson JG, Forsén T & Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002; 31: 1235-39.
2. Eriksson JG, Forsén T, Tuomilehto J, Osmon C & Barker DJP. Early growth and coronary heart disease in later life: longitudinal study. BMJ 2001; 322, 949-53.
3. National Committee on Breastfeeding. Breastfeeding in Ireland: A five-year strategic action plan. 2005; ISBN 0-9544914-4-0. The Department of Health and Children, Dublin.
4. Food Safety Authority of Ireland. Recommendations for a national infant feeding policy. Food Safety Authority of Ireland, Dublin. 1999. Available at: http://www.fsai.ie/resources_and_publications/nutrition_publications.html#Directory1.
5. Agostoni C, Decsi T, Fewtrell M, Goulet O, Kolacek S, Koletzko B, Fleischer Michaelson KF, Moreno L, Puntis J, Rigo J, Shamir R, Szajewska H, Turck D, van Goudoever J. Complementary Feeding: A commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2008; 46: 99-110.
6. Skinner JD, Carruth BR, Bounds W, Ziegler PJ. Children’s food preferences: a longitudinal analysis. J Am Diet Assoc. 2002; 102: 1638-47.
7. Tarrant RC, Younger KM, Sheridan-Pereira M, White MJ, Kearney JM. Factors observed with weaning practices in term infants: a prospective observational study in Ireland. Br J Nutr. 2010; 104: 1544-54.
8. Burdette HL, Whitaker RC, Hall WC, Daniels SR. Breastfeeding, introduction of complementary foods, and adiposity at 5 y of age. Am J Clin Nutr. 2006; 83: 550-8.
9. Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, Kelner CJ. Health consequences of obesity. Arch Dis Child. 2003; 88: 748-52.
10. Whelton H, Harrington J, Crowley E, Kelleher V, Cronin M, Perry IJ. Prevalence of overweight and obesity on the island of Ireland: results from the North South Survey of Children’s Height, Weight and Body Mass Index, 2002. BMC Public Health. 2007; 7: 187-95.
11. Fabricatore AN, Wadden TA. Psychological aspects of obesity. Clin Dermatol. 2004; 22:332-37
12. Wadden TA, Didie E. What’s in a name? Patients’ preferred terms for describing obesity. Obesity Research. 2003; 11:1140-46.
13. Maziak W, Ward KD, Stockton MB. Childhood obesity: are we missing the big picture? Obes Rev. 2008; 9: 35-42.
14. Flynn MAT, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, Tough SC. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’ recommendations. Obes Rev. 2006; 7: 7-66.
15. National Taskforce on Obesity. Obesity: The Policy Challenges. 2005. Available at: http://www.dohc.ie/publications/pdf/report_taskforce_on_obesity.pdf?direct=1.
16. Freeman VE, Mulder J, van’t Hof MA, Hoey HMV, Gibney MJ. A longitudinal study of iron status in children at 12, 24 and 36 months. PHN. 1998; 1: 93-100.
17. Carter RC, Jacobson JL, Burden MJ, Armony-Sivan R, Dodge NC, Angelilli ML, Lozoff B, Jacobson SW. Iron deficiency anemia and cognitive function in infancy. Pediatrics. 2010; 126: 427-34.
18. Iannotti LL, Tielsch JM, Black MM, Black RE. Iron supplementation in early childhood: health benefits and risks. Am J Clin Nutr. 2006; 84: 1261-1276.
19. Haase T, Pratschke J. An inter-temporal and spatial analysis of data from the Census of Population, 1991, 1996, 2002 and 2006 [Internet]. Managed by Pobal, Holles Street, Dublin. Published on behalf of the Department of Community, Equality and Gaeltacht Affairs. 2008. Available at: https://www.pobal.ie/WhatWeDo/Deprivation/Pages/AreaProfiles.aspx.
20. Brug J. Determinants of healthy eating: motivation, abilities, and environmental opportunities. Family Practice 2008; 25: i50-i55.
21. Brewis S, Gartin M. Biocultural construction of obesogenic ecologies of childhood: parent-feeding versus child-eating strategies. A J Hum Biol. 2006; 18: 203-13.

|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|