O Chukudebelu1, A Dias1, C Timon1,2
1Department of Otolaryngology, Head & Neck Surgery, Royal Victoria Eye & Ear Hospital, Adelaide Rd, Dublin 2
2Department of Otolaryngology, Head & Neck Surgery, St James’s Hospital, James’s St, Dublin 8
Abstract
The objective of this study was to establish the indications, referral trends and demographics for thyroidectomies performed in our institutions over a 13-year period by a single surgeon. We conducted a retrospective chart review of 1003 consecutive thyroidectomies at our institutions during the period 1998 until 2010. The parameters incorporated to this study were age, sex, county, referral source, symptoms, thyroid status, procedure performed, histopathology and post-operative complications. The age range of patients was 4-87 years. There were 777 females and 226 males, with a sex ratio of 3.4:1. The mean age was 51 years. The commonest indications for surgery were a potential or definite neoplastic thyroid mass (781 cases - 78%), compressive symptoms (119 cases - 12%), thyrotoxicosis and endocrine related causes (103 cases -10%). 896 (89.3%) patients were euthyroid, 4 (0.4%) hypothyroid and 103 (10.3%) hyperthyroid. There were 739 partial thyroidectomies and 264 total thyroidectomies. Histopathology results showed that 742 were benign and 261 malignant, of which papillary carcinomas accounted for 75.1%, follicular carcinomas 13.4%, Hurthle cell carcinoma 1.5%, medullary thyroid carcinomas 3 %, undifferentiated carcinomas 3 %, others (lymphoma and squamous cell carcinomas) 4%. Post-operative complications were: Temporary hypocalcaemia - 6.4%, Permanent hypocalcemia in -0.8 %. Haemorrhage and seroma in 1.5%, unilateral vocal cord paralysis in 1.2%, post-operative wound infection in 0.3% and pulmonary embolism in 0.01%. There was no mortality. Dublin accounted for 519 (51.7%) of referrals, 484 (48.3%) was from the rest of the country. General practitioners accounted for 84.8% of referrals. Endocrine referrals comprised 9.8%. Other specialities constituted 5.4 %. Two significant findings from this study were; firstly, a trend depicting increasing referral rates from the general practitioner and endocrine services. Secondly, low post-operative complication rates that compare favourably to published figures in previous studies from tertiary centres.
Introduction
Thyroid disease is thought to have undergone a real or perceived increase in incidence over the past 20 years. This has been attributed to a number of factors, namely; improved awareness of symptoms by the general population and the easy access to sophisticated diagnostic tools at the disposal of primary care physicians1,2,7. In the Irish health care setting, general practitioners are usually the first point of contact for patients with thyroid disease. Benign thyroid disease is routinely managed medically by general practitioners and physicians. Surgical management of thyroid disease is warranted in patients with failed medical control, compressive symptoms and neoplastic concerns. We undertook this study to determine local indications for surgery, patterns of referral and demographic trends for thyroidectomies performed in our institutions by the senior author over a 13-year period.
Methods
Patients who underwent a thyroidectomy at the Royal Victoria Eye & Ear Hospital, Dublin and St James Hospital, Dublin, were reviewed by the senior author and deemed eligible for inclusion to this study. We conducted a retrospective chart review on 1003 patients who had undergone a thyroidectomy between 1998 and 2010. The parameters incorporated in the study were patient age, sex, county, referring source, symptoms, thyroid status, procedure performed, histopathology and post-operative complications. We explored each parameter to detect trends and referral patterns that had undergone a change within the time period of the study.
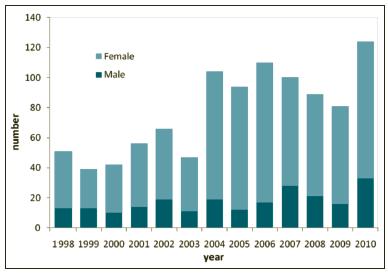
Figure 1: Demographics by sex 1998-2010
Results
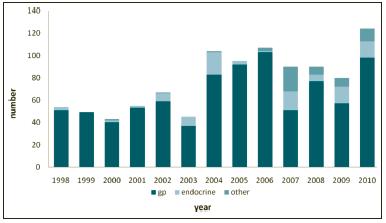
1003 thyroidectomies were performed by the senior author from 1998 to 2010 at the Royal Victoria Eye & Ear Hospital and St James Hospital, Dublin. The age range of patients was from 4-87 years with a mean age of 51 years. The mean age for females was 50 years (4-86) and 52 years for males (10-87). The sex ratio was 3.4:1, female – 77.5% (n=777), males -22.5% (n=226) (see Figure 1). The most common indications for surgery were a suspicion or definite neoplastic process in 781 patients (78 %), compressive symptoms in 119 (12%), thyrotoxicosis and endocrine causes in 103 cases (10%). Thyroid status was determined preoperatively in all patients. As you would expect 896 (89.3%) patients were euthyroid, 4 (0.4%) hypothyroid and 103 (10.3%) hyperthyroid. Referral sources were from General Practitioners – 84.8% (n=851), Endocrine Services – 9.8% (n=98), Otolaryngology – 2.4% (n=24), General Physicians - 0.4% (n=4), General Surgery – 2.0% (n=20), Oncology – 0.3% (n=3), Ophthalmology – 0.3% (n=3) (see Figure 2). We observed that there were significant increased referral rates over the 13 year period from the general practitioner and endocrine services. These were a 92% increase in referral rates from general practitioners for the year 2010 compared to 1998 and a 400% increase in referrals from Endocrine sources for the same period (see Figure 2).
Figure 2: Demographics by Referral Source 1998-2010
We conducted 739 partial thyroidectomies and 264 total thyroidectomies of which 14 patients also required a modified radical neck dissection. Five patients required a sternal split due to a large or inaccessible retrosternal goitre which was done in conjunction with our cardiothoracic colleagues. Mean operating times were 68 minutes for partial thyroidectomies (35-210 minutes SD 23.78) and 78.5 minutes for total thyroidectomies (38-210 minutes SD 42.18). Since 2005 drains were used in 15 cases -14.9%.
Figure 3: Per cent frequency Distribution of Patient Demographics by Histology; Thyroid Carcinoma
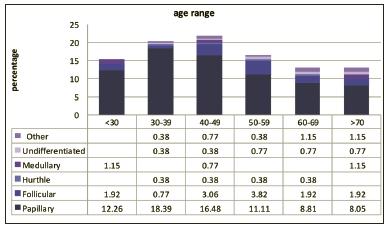
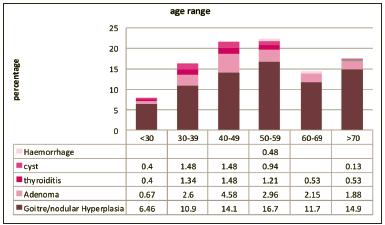
Histopathology reports showed 742 patients (74%) to have benign thyroid disease. There were 600 females and 142 males with benign disease. The female to male ratio for patients with benign thyroid disease was 4.2:1. The mean age of patients with benign thyroid disease was 50 years. The mean age was 40 years for females (16-87) and 60 for the male patients (19-84). 261 patients (26%) had a thyroid malignancy. The vast majority were thyroid papillary carcinomas which occurred in 196 patients (75.1%). Female to male ratio for patients with a papillary carcinoma was 2.7:1. The mean age for females with a papillary carcinoma was 43 years (29-78 years). 8 females had a metastatic papillary carcinoma at initial presentation. The mean age for females with metastatic disease was 47 years. The mean age for males with a papillary carcinoma was 47.6 years (20-81 years). Of this number, nine had metastatic disease.
The mean age for males with metastatic disease was 48 years.
Follicular carcinomas occurred in 35 patients, accounting for 13.4 % of thyroid carcinomas. The female to male sex ratio was 2:1. The mean age for all patients with a follicular carcinoma was 53 years. These were 55.4 years in females and 50.3 years in males. Hurthle cell carcinomas occurred in 4 patients -1.5%, medullary thyroid carcinomas in 8 patients - 3%. Undifferentiated thyroid carcinomas in 8 patients - 3%. Other carcinomas (Lymphoma and squamous cell carcinoma) occurred in 10 cases - 4 %. Post-operative complications were a transient hypocalcaemia as defined by serum calcium dropping below 2.0 mmol, or symptomatic patients requiring calcium supplementation on discharge9. 19 of 264 patients undergoing total thyroidectomy had hypocalcemia-7.2%. Permanent hypocalcaemia requiring calcium supplementation for over six months occurred in 2 of 264 patients-0.8%. Post-operative haemorrhage and seroma requiring surgical intervention occurred in 1.5% of patients (n=15). Unilateral vocal cord paralysis occurred in 1.2% (n=12). These were associated with nine total thyroidectomies and three partial thyroidectomies. There was no bilateral vocal cord paralysis. Post-operative wound infection rates were 0.3%, and pulmonary embolism occurred in 0.01%.
Figure 4: Per cent frequency Distribution of Patient Demographics by Histology; Benign Thyroid Disease
Discussion
In one recently published article, Gourin et al reported “significantly increased proportions of thyroid surgical procedures performed by high-volume surgeons and in high-volume hospitals”3. These trends are consistent with the findings from our study .To provide a rationale for this in our setting; we postulate that a combination of factors could explain the trend. Foremostly, there has been a shift towards subspecialty appreciation, with an increased emphasis on the role of the head and neck surgeon in the management of surgical thyroid disease within the past decade5,6. In our institutions this has become evident in increased referral rates especially from the general practitioner and endocrine services. Secondly these trends may in part be attributable to an enhanced public awareness of the symptoms and signs of thyroid disease. This could be an indirect consequence of an expansion in information through the electronic media. A third consideration is the increasingly sophisticated diagnostic tools, particularly with respect to diagnostic imaging devices readily available at the disposal of general practitioners2.
In our study general practitioners constituted the overall majority of referrals to our hospitals, constituting 84.8 % of all patients admitted to our institutions for a thyroid surgery. There was a 92 % increase in referral rates from general practitioners to our units for the year 2010 as compared to 1998. Endocrine referrals constituted 9.8 % of referrals to our units. There was a 400% increase in rates of referral from endocrine services for the year 2010 as compared to 1998. Other specialities made up 5.4% of all referrals to our services (see Figure 2). The average age of patients in our study was 51 years with an overall female preponderance (77.5%). There was a wide spectrum in ages from 4-87 years. The youngest patients in our study to undergo surgery were a group of patients aged 4-10 years who had the proto-oncogene for medullary thyroid carcinoma and these underwent a prophylactic total thyroidectomy. Our data clearly showed that the most common indications for thyroid surgery were a potential or definite neoplastic thyroid mass-78 % compressive symptoms -12%, and endocrine causes -10%.These findings compare favourably with previously published studies. In their article Bhattacharyya et al identified a mean age of 48.3 years. The most common indication for surgery in their study was for a thyroid malignancy and goitre (73.9%)4.
County demographics in our study were a reflection of our location which is Dublin. Over half of referrals were from Dublin, whilst the remainder were from the rest of the country underscoring the high volume and tertiary referral nature of our hospitals. In our institutions, we place emphasis on adherence to standard departmental protocols in the evaluation of all patients who undergo a thyroid surgery. Upon receipt of a referral, all patients undergo a preliminary evaluation which incorporates outpatient clinic appointments, a thyroid function assessment, multidisciplinary team review and fine needle aspirate cytology in suspected neoplasia, together with imaging and preoperative functional vocal assessment in all patients. Intraoperative recurrent laryngeal nerve monitors are utilised in all cases. Special attention is paid to the parathyroid glands which are carefully identified and preserved. Drains were utilised routinely up until 2004. However, we now only adopt the use of drains in select cases with significant haemorrhage as we did not find any significant benefit to their continued routine use. Recorded usage of drains since 2005 was 15 patients- 14.9%.
We observed for trends with respect to post-operative complications. Hypocalcaemia (defined by serum calcium dropping below 2.0 mmol/L) or a symptomatic hypocalcaemia requiring calcium supplementation (rates of 1-40% in the literature)4,11,12 and a unilateral or bilateral recurrent laryngeal nerve injury (rates of 1-3% in the literature).4,10 Our low post-operative complications rates are a reflection of high volume surgeon experience on the part of the senior author and emphasis on strict adherence to standard departmental protocols. In their article, Sosa et al stressed the importance of surgeon volume and outcomes13. In our study unilateral vocal cord paralysis occurred in 1.2% of patients. There was no bilateral vocal cord paralysis. Hypocalcaemia occurred in 7.2% patients undergoing a total thyroidectomy. Permanent hypocalcaemia requiring calcium supplementation for over six months occurred in two of these patients -0.8%. Post-operative haemorrhage and seroma requiring surgical intervention occurred in 1.5% of our patients. Our postoperative wound infection rates were 0.3%, and pulmonary embolism occurred in 0.01%. We did not record any post-operative mortality. These figures compare favourably to published figures from other tertiary centres. In their study Bhattacharyya et al reported unilateral and bilateral vocal cord paralyses rates of 0.77% and 0.39% respectively; their incidence of postoperative hypocalcaemia was 6.2%, postoperative wound haematoma 1.0%, wound infection 0.2%, and mortality rate was 0.2%4.
The findings of our study suggest that we anticipate and plan for a closer liaison between endocrine units, general practitioners, allied services and head and neck units. As the trend depicts increasing referrals rates, we should accordingly anticipate for a closer collaboration between these specialities and the head and neck surgeon. We would encourage further studies on prevalence of thyroid disease in Ireland.
Correspondence: O Chukudebelu
Department of Otolaryngology, Head & Neck Surgery, St James’s Hospital, James’s St, Dublin 8
Email: [email protected]
References
1. Canaris GJ, Manowitz NR, Mayor G, et al. The Colorado Thyroid Disease Prevalence Study. Arch Intern Med. 2000;160:526-534.
2. Davies L, Welch HG. JAMA. Increasing incidence of thyroid cancer in the United States, 1973-2002. 2006 May 10;295:2164-7.
3 Gourin CG, Tufano RP, Forastiere AA, Koch WM, Pawlik TM, Bristow RE. Volume-based trends in thyroid surgery.Arch Otolaryngol Head Neck Surg. 2010 Dec;136:1191-8.
4. Bhattacharyya N, Fried MP. Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg. 2002;128:389-392.
5. Ramsden JD, Johnson AP, Cocks HC, Watkinson JC. Who performs thyroid surgery: a review of current otolaryngological practice. Clin Otolaryngol Allied Sci. 2002 Oct;27:304-9.
6. Terris D J,Seybt M W, Siupsinskiene N, Gourin C, Chin E.Thyroid surgery changing patterns of practice . Laryngoscope 116: June 2006 911-915.
7. A Chen ,A Jemal , E M Ward ,Increasing incidence of Differentiated Thyroid Cancer in the United States, 1988-2005 Cancer 2009; 3801-3807
8. Pareschi R, Mincione A, Destito D, Mola M, Righini S, Assi A, Dottorini M. Surgery of thyroid cancer: twelve years' personal experience. Acta Otorhinolaryngol Ital. 2004 Dec;24:348-53
9. Wong C, Price S, Scott-Coombes D. Hypocalcaemia and parathyroid hormone assay following total thyroidectomy: predicting the future. World J Surg. May 2006;30:825-32. [Medline].
10. Pappalardo G, Guadalaxara A, Frattaroli FM, Illomei G, Falaschi P. Total compared with subtotal thyroidectomy in benign nodular disease: personal series and review of published reports. Eur J Surg. 1998;164:501-506.
11. Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP. Morbidity of thyroid surgery. Am J Surg. 1998;176:71-75.
12. Flynn MB, Lyons KJ, Tarter JW, Ragsdale TL. Local complications after surgical resection for thyroid carcinoma. Am J Surg. 1994;168:404-407.
13. Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R.The importance of surgeon experience for clinical and economic outcomes from thyroidectomy.Ann Surg. 1998 Sep;228:320-30.
14. Lamadé W, Renz K, Willeke F, Klar E, Herfarth C.Effect of training on the incidence of nerve damage in thyroid surgery. Br J Surg. 1999 Mar;86:388-91
15. Prim MP, De Diego JI, Hardisson D, Madero R, Gavilan J. Factors related to nerve injury and hypocalcemia in thyroid gland surgery. Otolaryngol Head Neck Surg. 2001;124:111-114.
16. Vincent G.Thyroidectomy over a quarter of a century in the Belgian Ardennes: a retrospective study of 1207 patients.Thyroid. 2001 Feb;11:187-92.
17. Werga-Kjellman P, Zedenius J, Tallstedt L, Träisk F, Lundell G, Wallin G. Surgical treatment of hyperthyroidism: a ten-year experience.Acta Chir Belg. 2008 Sep-Oct;108:542-7.
18. Mitchell I, Livingston EH, Chang AY, Holt S, Snyder WH 3rd, Lingvay I, Nwariaku FE Trends in thyroid cancer demographics and surgical therapy in the United States. Eur Arch Otorhinolaryngol. 2011 Jun;268:899-906. Epub 2010 Nov 12.
19. Olaleye O, Ekrikpo U, Moorthy R, Lyne O, Wiseberg J, Black M, Mitchell D.Increasing incidence of differentiated thyroid cancer in South East England: 1987-2006.Laryngoscope. 2006 Jun;116:911-5.
20. Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP. Am J Surg. 1998 Jul;176:71-5.Morbidity of thyroid surgery. Department of Visceral Surgery, Angers University Hospital, France.
21. Prim MP, de Diego JI, Hardisson D, Madero R, Gavilan J. Factors related to nerve injury and hypocalcemia in thyroid gland surgery.Otolaryngol Head Neck Surg. 2001 Jan;124:111-4.
22. Herranz-González J, Gavilán J, Matínez-Vidal J, Gavilán C. Complications following thyroid surgery.Arch Otolaryngol Head Neck Surg. 1991 May;117:516-8.
