|
|
|
|
|
|
|
|
M McDonnell Naughton,C McGarvey,Myra O'Regan,TG Matthews
|
|
|
|
Ir Med J. 2012 Apr;105(4):105-8
|
|
M McDonnell/Naughton1, C McGarvey2, M O’Regan3, T Matthews2
1Department of Nursing and Health Science, Athlone Institute of Technology, Co Westmeath
2National Sudden Infant Death Register, The Children’s University Hospital, Temple St, Dublin 1
3Department of Statistics, Trinity College, Dublin 2
Abstract
A population based case control study was conducted to examine alcohol consumption and maternal smoking during pregnancy and the risk of SIDS in an Irish population. Each SIDS case (n=287) was compared with control infants (n=832) matched for date and place of birth for infants born from 1994 to 2001. Conditional logistic regression was used to investigate differences between Cases and Controls establishing Odds Ratio’s (OR) and 95% Confidence Intervals (CI). Mothers who smoked were 3 times more likely to have a SIDS Case, and a dose response effect was apparent, with mothers smoking 1-10 cigarettes/day OR 2.93 (CI 1.50-5.71), and those smoking >10 cigarettes/day OR 4.36 (CI 2.50-7.61). More Case mothers consumed alcohol during pregnancy than Control mothers and, within drinkers, the amount of alcohol consumed was also greater (p<0.05). A dose response with frequency of drinking was apparent. The adjusted odds ratio for those consuming alcohol in all three trimesters was 3.59 (CI:1.40-9.20). Both of these risk factors are modifiable and need to be incorporated into antenatal education from a SIDS point of view.
Introduction
SIDS is a major cause of infant mortality in the Western world with a rate of 0.37 per 1,000 live births in Ireland currently.1 The Reduce the Risks of SIDS Campaign ran nationally and internationally over the past 18 years, was successful in reducing the SIDS rate. In Ireland the rate fell from 2.2/1000 live births in the 1980’s to 0.37/1000 live births currently, resulting in the greatest improvement in infant mortality in 30 years to under 4/1000 live births, since 2006 the equivalent of approximately 100 fewer infant deaths per year.1 The aim of this study was to review alcohol consumption and maternal smoking during pregnancy and to investigate whether they are risk factors for SIDS.
Methods
This study was part of a population based case control study of SIDS in the Republic of Ireland. The National Sudden Infant Death Register is notified of all sudden unexpected infant deaths (SUDI) in Ireland, usually within 48hrs of occurrence. Of these, all cases occurring between the 1st January 1994 and 31st December 2003 with ‘SIDS’ as the certified cause of death were included. A SIDS Case was defined as the sudden death of an infant or young child where, following a thorough post mortem examination, no cause was found for the death (Beckwith 1970 definition).2
Four controls were selected randomly from the birth register and matched for date of birth and the same community care area as the index case. Both case and control families were invited by letter to participate in a home interview which was conducted on average within six weeks of the index case’s death. A detailed account of recruitment and interview processes has previously been described by Matthews’s et.al. (2004).3 The Department of Health and Children approved the study and consent was obtained from parents to participate in the research. The average age of cases at time of death was 17.6 weeks and average age of control infants at interview was 25.3 weeks. All univariate analysis of variables related to the infants’ last sleep was adjusted for this age difference by inclusion of a variable for infant age in the logistic regression analysis. SIDS cases were notified to the SIDS Register, as previously described.3,4 The parental questionnaire was designed to collect detailed information in several issues, including the following: socio-demographic data; pregnancy and birth; infant’s medical history; environmental characteristics; current child care parenting practices, lifestyle practices, including the use of cigarettes, alcohol and drugs, and details of events in the 48 hours preceding the infant’s death inclusive of the exact sleeping arrangements of the baby both during the baby’s lifetime and for the last sleep period.
A binary variable for ‘parental alcohol consumption in last sleep’ was constructed based on a Yes/No answer to the question, ‘did you consume alcohol (any quantity), during this pregnancy?’. For individuals that answered ‘yes’, additional questions were posed in relation to the weekly quantity consumed, subsequently converted to units by the researchers, for each trimester in turn. A social disadvantage index, scoring 0-5 (5=most deprived), was devised by adding a score of 1 for each of the following; having a medical card (a low income based free health service entitlement), being in public rented accommodation, not owning a car, household unemployment (i.e. both parents unemployed) and mother on social welfare. Individuals scoring >=3 were categorised as disadvantaged, coded as 1 vs 0 for scores 0-2 in the binary variable. A continuous variable was created for Z scores of weight by gestation (multiples of standard deviations from the normal mean) by relating the birth weight of each baby to controls of similar gestation. These scores were adjusted for the effects of gender and parity on birth weight. Computer generated norms compiled in the UK were used since norms for Ireland were not available and were adjusted for the effects of gender and parity on birth weight.5
The variable ‘history of illness since birth’ referred to any symptoms or illness experienced by the infant during his/her lifetime. Continuous variables for ‘combined tog value of infant clothing and bedding during the last sleep period’, maternal age and number of previous live born children were modified to derive binary variables with tog <10 (0) vs tog>=10 (1), maternal age >=25yrs (0) vs <25yrs (1) and <3previous live births (0) vs. >=3previous live births (1). The variable ‘co-sleeping during the last sleep’ was defined as any shared sleeping arrangement of an infant with an adult in or on a bed/sofa/armchair while ‘bed-sharing’ refers to infants sharing an adult bed with one or more adults. Infants who were room-sharing but not bed or sofa sharing were not included in the definition for co-sleeping. Other variables were ‘yes/no’ answers to questions relating to sociodemographics, mother’s pregnancy, and infant health during their lifetime as well as the 48hrs prior to death and finally the last sleep period. A reference sleep period occurring during the same time of day as the case infant’s last sleep was used for controls, where sleep period 1 = 08:00-11:59, sleep period 2 = 12:00-17:59, sleep period 3 = 18:00-21.59 and sleep period 4 = 22:00-07:59.
Conditional logistic regression was used, to investigate differences between cases and controls with respect to a number of potential risk factors using the statistical package Stata version 11. Odds ratios, 95% confidence interval levels and P values were calculated to express results. Each variable was examined in a univariate analysis before being adjusted for potential confounding factors in a multivariate analysis. The multivariate analysis was carried out using an additive stepped approach with variables introduced into the model in a sequence of time determined stages starting with pre-pregnancy variables and progressing through history of prior pregnancies, variables related to the current pregnancy, birth related variables, post delivery issues, the week prior to death, the 48 hours before death and the last/reference sleep period. Criteria for inclusion in the multivariate model having achieved statistical significance at univariate level (P<0.05) and having not greater than 10% of values missing. Data was not provided for every variable in each case which accounts for the variation in proportions of subjects from one variable to the next. Data may be accepted as missing at random. Differences between median values for continuous variables for alcohol consumption during pregnancy were examined using Wilcoxon’s rank sum test.
Results
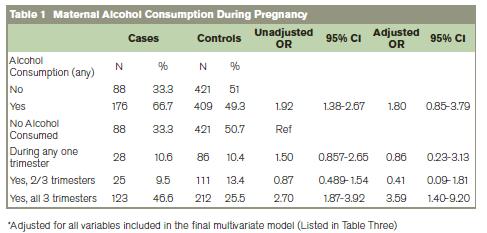
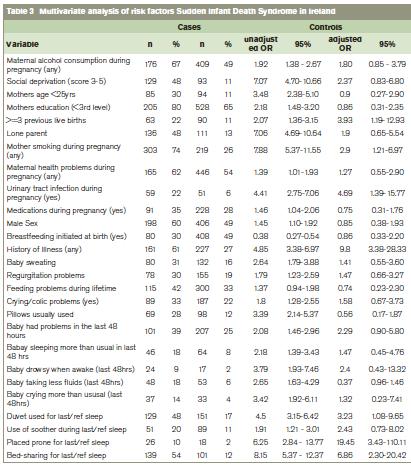
A total of 287 Case families agreed to participate in the study, corresponding to a response rate of 86% with 198 male (69%) and 89 female (31%) and of these 276 families completed the questionnaire. An average of three Control families per Case that responded to initial contact agreed to participate, (a response rate of 86% (832/966) with 406 (48.9%) males and 426 (51.1%) females. A significantly greater proportion of case mothers (67%) consumed alcohol during pregnancy than controls (49%) (Table 1). On multivariate analysis the OR associated with the variable for any maternal alcohol consumption was not statistically significant (Table 1). However when stratified by consumption per number of trimesters, alcohol consumption during all three but not one or two trimesters of pregnancy was found to be significantly increase the risk of SIDS with an adjusted OR of 3.59 (Table 1).
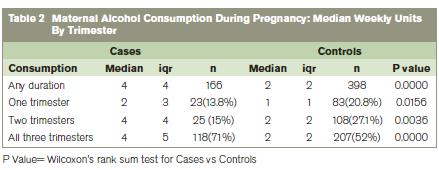
The median weekly units of alcohol consumed by case mothers during pregnancy was significantly more than that of controls (Table 2). When stratified by number of trimesters for which alcohol was consumed, in each case, the median number of units consumed by case mothers was significantly more than that of controls. For any duration of pregnancy the median units of alcohol consumed by Cases was 4 versus 2 for the controls (P<0.001). For each trimester/combination of trimesters case mothers consumed significantly more units than controls and this difference was particularly apparent for mothers that drank during all three trimesters (P value <0.0001). In relation to smoking 74% of case mothers smoked during pregnancy versus 26% of controls (OR 2.9; 95% CI: 1.21–6.97) with a dose response effect apparent with the risk of SIDS in the 1-10 cigarettes per day group (OR 2.93; 95% CI 1.50-5.71) rising in the >10 cigarettes/day group (OR 4.36; CI 2.50-7.61). This evidence of a dose response effect is supportive of a causal role of smoking.9 Misclassification of exposure to smoking in studies is possible.10
Continuous variable for z scores of birthweight adjusted for gestation, primgravida and gender included in the multivariate analysis.
Discussion
This study reconfirms previously identified risk factors for SIDS with smoking still the major modifiable risk factor.3,4,7 Health professionals need to act on this public health challenge. The risk associated with maternal smoking is increased substantially if the infant bed shares.10-12 Smoking may have consequences beyond the perinatal period.13,14 This study validates that difficult social circumstances are associated with SIDS.6,8 Reducing the SIDS risk by changing levels of social deprivation, is not easily amenable to health educational messages. Alcohol use while pregnant has emerged as a significant SIDS risk factor when consumed through all three trimesters of pregnancy with 67% of SIDS mothers consuming alcohol while pregnant compared to 49% of the control group, which replicates previous findings that alcohol consumption during pregnancy is a contributing factor to SIDS.14-17 The average weekly units of alcohol consumed by case mothers was significantly greater than that of control mothers; 5.4units/week vs 2.49 (P<0.001). Examination of the effect of number of units consumed weekly displayed a dose response effect in the univariate analysis. However, regardless of the categorisation used, ORs associated with all categories were not significant when variables for the last sleep were included in the multivariate analysis. Examination of data on alcohol consumption by trimester during which consumption occurred indicated a significant risk, but only when consumption was conducted throughout the pregnancy. Most Reduce the Risks of SIDS campaigns have successfully focussed on placing babies on their backs to sleep.8,10 Antenatal advice should incorporate abstaining from alcohol consumption while pregnant.
The study although retrospective is a valuable population study. A grieving family, although very emotional can recall accurately those events relating to the death. The family was dealt with sensitively. It is impossible to remain a detached observer.18 Self-selection may bias results. However, analysis of socio-demographic data on responders and non-responders showed no major differences. Interviews were similarly carried out which ensured uniformity of application with all social classes represented in the study. Although it is not always possible in any study to eliminate systematic bias, the safety measures taken in this study by the design, conduct and analysis of the work have attended to such concerns in detail and thus allow the results to be accepted.
Acknowledgements
Thanks to all the families who gave so generously of their time and participated in this study.
Correspondence: M McDonnell-Naughton
Department of Nursing and Health Sciences, Athlone Institute of Technology, Dublin Road, Athlone, Co Westmeath
Email: [email protected]
References
1. Matthews T, McGarvey C, Hamilton K. Annual Reports 2007, 2011; Dublin: Irish Sudden Infant Death Register, St. Georges Hall Temple St. University Hospital, 2007, 2011.
2. Beckwith JB. Discussion of Terminology and Definition of the Sudden Infant Death Syndrome. Ithaca, NY: Perinatology Press. In: Bergman AB, Beckwith JB, Ray CG, eds. Proceedings of the second international conference on causes of sudden deaths in infants. Seattle: University of Washington Press, 1970a: 14-22.
3. Matthews TG, McDonnell M, McGarvey C, Loftus G, O’Regan M. Multivariate “time based” analysis of SIDS risk factors. Arch Dis Child; 2004:89; 267-271.
4. McGarvey C, McDonnell M, Hamilton K, O’Regan M, Matthews T. An eight year study of risk factors for SIDS; Bed sharing versus non bed sharing. Arch Dis Child; 2006; 91: 316-323.
5. Tin W, Wariyar UK, Hey EN. Selection biases invalidate current low birthweight weight-for-gestation standards. The Northern Neonatal Network. British Journal of Obstetrics and Gynaecology 1997; 104: 180–185.
6. Whelan, C. “Welfare Regime and Social Class Variation in Poverty and Economic Vulnerability in Europe: An Analysis of EU-SILC. Journal of European Social Policy 2010: 20:316-332.
7. Blair PS, Nadin P, Cole TJ, Fleming PJ, Smith IJ, Platt MW, Berry PJ, Golding J. Weight gain and sudden infant death syndrome: changes in weight z scores may identify infants at increased risk. Archives of Disease in Childhood 2000; 82: 462-469.
8. Vennemann MM, Findeisen M, Butterfass-Bahloul T, Jorch G, Brinkmann B, Kopcke W, Bajanowski T, Mitchell EA; The GeSID Group. Modifiable risk factors for SIDS in Germany: results of GeSID. Acta Paediatr. 2005 94: 655-60.
9. Lesko SM, Corwin MJ, Vezina RM, Hunt CE, Mandell F, McClain M, Heeren T, Mitchell AA. Changes in sleep position during infancy: a prospective longitudinal assessment. JAMA 1998; 280: 329-35.
10. Carpenter RG, Irgens LM, Blair PS, England PD, Flemin, P, Huber J, Jorch G, Schreuder, P. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet 2004; 363: 185-91.
11. Tappin D, Ecob R, Brooke H. Bedsharing, roomsharing, and sudden infant death syndrome in Scotland: a case-control study. The Journal of Pediatrics. 2005; 147: 32-7.
12. McDonnell M, Mehanni M, McGarvey C, O’Regan M, Matthews TG. Smoking: the major risk factor for SIDS in Irish infants. Irish Medical Journal 2002; 95: 4: 111-113.
13. Mitchell E.A, Hutchinson L, Stewart AW. The continuing decline in SIDS mortality Archives of Disease and Childhood 2007; 92: e7.
14. Daltveit AK, Irgens LM, Oyen N, Skjaerven R, Markestad T, Alm B, Wennergren G, Norvenius G, Helweg-Larsen K. Sociodemographic risk factors for sudden infant death syndrome: associations with other risk factors. The Nordic Epidemiological SIDS Study. Acta Paediatrica 1998; 87: 284-290
15. Friend K., Goodwin MS., Lipsett LP. Alcohol use and Sudden Infant Death Syndrome 2004.www.Alcohol use and sudden infant death syndrome.com accessed Dec 2010.
16. L’Hoir M, Engelberts A, van Well G, Bajanowski T, Helweg-Larsen K, Huber J. Sudden unexpected death in infancy: epidemiologically determined risk factors related to pathological classification Acta Paediatrica 1998; 87: 1279–1287.
17. Faden, Graubard & Dufour 1997 The relationship of drinking and birth outcome in a US national sample of expectant mothers Paediatric and Perinatal Epidemiology: Volume 11: 167–180.
18. Fleming P, Blair P, Bacon C, Berry J. Sudden unexpected deaths in infancy: the CESDI SUDI Studies 1993-1996. London: Stationery Office, 2000.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|