|
|
|
|
|
|
|
|
R Woods,JO Larkin,C Muldoon,MJ Kennedy,B Mehigan,P McCormick
|
|
|
Ir Med J. 2012 Mar;105(3):88-9
R Woods, JO Larkin, C Muldoon, MJ Kennedy, B Mehigan, P McCormick
St James’s Hospital, James’s St, Dublin 8
Abstract
A 16 year old girl presented to our unit with crampy abdominal pain, change in bowel habit, a subjective impression of weight loss and a single episode of haematochezia. She was found to have a rectosigmoid adenocarcinoma and proceeded to laparoscopic anterior resection, whereupon peritoneal metastases were discovered. She received chemotherapy and is alive and well ten months later with no radiological evidence of disease. Colorectal carcinoma is rare in the paediatric population but is increasing in incidence. Early diagnosis is critical to enable optimal outcomes.
|
Introduction
Colorectal carcinoma is relatively rare in the paediatric patient with only 1% of all cases occurring in children1. Nonetheless, the disease is increasing in overall incidence and the often late diagnosis allied to frequently aggressive tumour biology equate to an overall poor prognosis. We report the case of a 16 year old girl with signet ring cell rectosigmoid carcinoma and discuss the literature relating to paediatric colorectal cancer.
Case Report
A 16 year old girl was referred to our outpatient clinic with a four week history of crampy abdominal pain, change in bowel habit, a subjective impression of weight loss and a single episode of haematochezia. She was previously well with no family history of colorectal carcinoma although her paternal aunt and grandmother had Crohn’s disease. Physical examination was unremarkable. Haematological and biochemical investigations were normal and Carcinoembryonic Antigen (CEA) was less than 1 ng/ml. Colonoscopy showed an irregular, impassable circumferential lesion, confirmed on rigid sigmoidoscopy to be at 13cm. Biopsies showed poorly differentiated signet ring adenocarcinoma positive for Cytokeratins 7 and 20. Computed tomography (CT) and magnetic resonance imaging (MRI) showed mural thickening at the rectosigmoid junction staged as T3N0 with a small amount of free fluid in the pelvis and no evidence of metastasis (Figure 1).
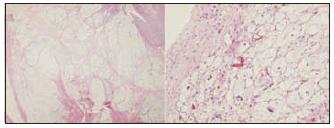
Following discussion at a multidisciplinary meeting, she underwent laparoscopy, where peritoneal carcinomatosis was noted, with extensive tumour plaques present in the pouch of Douglas. A palliative anterior resection was carried out. Histopathology showed poorly differentiated signet ring adenocarcinoma of the rectosigmoid junction, with a high degree of lymphovascular invasion, serosal involvement, metastatic involvement of 23 of 43 nodes and confirmed peritoneal metastases leading to a staging of pT4a pN2b pM1 (Figure 2). The appendix was also removed and was histologically normal. Following an uneventful postoperative recovery the patient commenced a course of palliative chemotherapy with Folinic acid, 5-Fluorouracil, Oxaliplatin and Bevacizumab (Folfox and Avastin). She is alive and well ten months postoperatively with no evidence of local disease recurrence or distant metastatic disease on follow-up CT.
Figure 1: axial CT image showing circumferential rectosigmoid mass
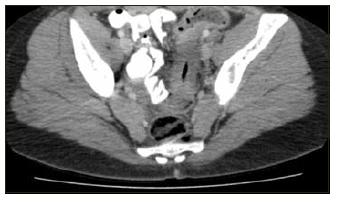
Figure 2 – H&E stain x20 of (a) primary tumour showing poorly differentiated signet ring adenocarcinoma replacing the mucosa, submucosa and muscularis propria, positive for Cytokeratins 7 and 20 and which was diastase-pretreated periodic acid-Schiff (DPAS) stain positive and (b) metastatic peritoneal deposit
Discussion
Recent trends suggest that the incidence of rectal and rectosigmoid cancer is increasing in patients aged under forty while the incidence of colon cancer remains largely static2. Underestimating this incidence may result in a failure to diagnose younger patients with rectal cancer in a timely manner. The disease carries an unfavourable prognosis with a 5 year survival of 40% in one Italian series (23% in those aged under 18)3, mainly due to greater incidence of more aggressive histotypes of signet ring cell or mucinous adenocarcinoma (40%) in comparison with 11% in adults4 and often a more advanced stage at presentation, in part due to delayed diagnosis in paediatric cases5. It is also likely that tumour biology differs between these cohorts6. There is evidence that sporadic colorectal carcinoma in children differs from cancers linked to familial adenomatous polyposis and hereditary nonpolyposis colorectal cancer and from adult colorectal carcinoma7.
Due to the limited number of cases of paediatric colorectal adenocarcinoma, a separate approach to treatment has not been defined and management is extrapolated from the approach to adult disease8. Case reports of paediatric colorectal carcinoma seem to universally follow adult treatment regimens while decrying the lack of a multi-centre study into appropriate strategies for the paediatric patient9. Notwithstanding the rarity of paediatric colorectal carcinoma, the disease is increasing in incidence and the predominantly aggressive tumour biology equates to an overall poor prognosis. Therefore, in order to reduce potential mortality, patients presenting with rectal bleeding or other cardinal features of colorectal cancer should be evaluated urgently, irrespective of age.
Correspondence: JO Larkin
Ardaulin, Carrick Rd, Dundalk, Co. Louth
Email: [email protected]
References
1. Shankar A, Renaut AJ, Whelan J, Taylor I.Colorectal cancer in adolescents. Ann R Coll Surg Engl. 1999; 81: 100-104.
2. Meyer JE, Narang T, Schnoll-Sussman FH, Pochapin MB, Christos PJ, Sherr DL. Increasing incidence of rectal cancer in patients aged younger than 40 years: an analysis of the surveillance, epidemiology, and end results database. Cancer. 2010 Sep 15;116:4354-9.
3. Ferrari A, Rognone A, Casanova M, Zaffignani E, Piva L, Collini P, Bertario L, Sala P, Leo E, Belli F, Gallino G. Colorectal carcinoma in children and adolescents: the experience of the Istituto Nazionale Tumori of Milan, Italy. Pediatr Blood Cancer. 2008 Mar;50:588-93.
4. Sultan I, Rodriguez-Galindo C, El-Taani H, Pastore G, Casanova M, Gallino G, Ferrari A. Distinct features of colorectal cancer in children and adolescents: a population-based study of 159 cases. Cancer. 2010 Feb 1;116:758-65.
5. Kravarusic D, Feigin E, Dlugy E, Steinberg R, Baazov A, Erez I, Lazar L, Kapuller V, Grunspan M, Ash S, Freud E. Colorectal carcinoma in childhood: a retrospective multicenter study. J Pediatr Gastroenterol Nutr. 2007 Feb;44:209-11.
6. Hill DA, Furman WL, Billups CA, Riedley SE, Cain AM, Rao BN, Pratt CB, Spunt SL. Colorectal carcinoma in childhood and adolescence: A clinicopathological review. J Clin Oncol. 2007;25:5808-14.
7. Datta RV, LaQuaglia MP, Paty PB. Genetic and Phenotypic Correlates of Colorectal Cancer in Young Patients. N Engl J Med. 2000;342:137-138.
8. Saab R, Furman WL. Epidemiology and management options for colorectal cancer in children. Paediatr Drugs. 2008;10:177-92.
9. Sultan I, Rodriguez-Galindo C, El-Taani H, Pastore G, Casanova M, Gallino G, Ferrari A. Distinct features of colorectal cancer in children and adolescents: a population-based study of 159 cases. Cancer. 2010 Feb 1;116:758-65.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|