|
|
|
|
|
|
|
|
A O'Farrell,D De La Harpe,H Johnson,K Bennett
|
|
|
|
Ir Med J. 2011 Sep;104(8):245-8
|
|
A O'Farrell1, D De La Harpe1, H Johnson2, K Bennett3
1Health Intelligence Unit, Health Service Executive, Palmerstown, Dublin 20
2Health Information Unit, Health Intelligence Ireland, Steevens’ Hospital, Dublin 8
3Department of Pharmacology & Therapeutics, Trinity Centre for Health Sciences, St James's Hospital, Dublin 8
Abstract
Chronic obstructive pulmonary disease (COPD) is one of the leading causes of mortality. Although more prevalent in men, it is anticipated that, due to the convergence in smoking rates, the prevalence rate in women will surpass that of men. There were 14,519 deaths attributable to COPD in the period 2000-2009. Although deaths decreased for both sexes, reduction in deaths was significantly higher among men (test for trend, p<0.01 for men vs. p=0.06 for women). Smoking rates decreased for both sexes from 1980-2009 with the percentage reduction in smoking significantly greater in men (11.5% vs. 7.0%, p<0.001). There has been a convergence in COPD deaths and COPD hospital in-patient discharges for men and women that mirrors the trend in the convergence of male and female smoking rates. This study provides evidence of the need for effective smoking cessation programmes that are targeted at women as well as men.
Introduction
Chronic obstructive pulmonary (COPD) disease is a general term for a number of chronic lung disorders also referred to as chronic bronchitis, emphysema, chronic obstructive airway disease and chronic airway flow limitation. It is a serious yet largely preventable and treatable chronic disease. COPD is one of the leading causes of mortality and morbidity worldwide.1 The prevalence of COPD in Ireland is unknown but based on international figures it is estimated that at least 400,000 people in Ireland have COPD of whom over 180,000 have moderate or severe disease.2 COPD prevalence also increases with age and it is estimated that it increases from approximately 10% of the population aged 40-49 years to over 50% in those aged 70 years or over.1,2 It is estimated that the Irish population aged over 35 years will increase by between 40-50% in the next 20 years and the major growth will be seen in those aged 50 years and over.4
Thus the burden of COPD on health services is expected to increase in the future. The main risk factor for COPD is smoking; it is estimated that between 50-85% of cases of COPD can be attributable to either current or previous smoking.5 Although the disease is more prevalent in men, it is hypothesized that, due to the convergence in male and female smoking rates, the rates of COPD among women will surpass those of men in around 10 years.6 This is because womens’ rates of tobacco use have typically lagged behind and peaked later than mens’ rate of smoking. Furthermore, studies have shown that women are more susceptible to COPD in response to smoking when exposed to the same amount of exposure to tobacco as men, and women are more likely to develop more severe and earlier on-set COPD than men.7-10
The prevalence of COPD has not previously been measured in Ireland as there are no registers available to record COPD incidence or prevalence. However, the use of health care resources in acute hospitals (e.g. hospital in-patient discharges) provide some measure of the prevalence of COPD although this will under-estimate the true prevalence of COPD in the community since patients admitted to acute hospitals usually have acute exacerbations of the disease and therefore present with later stage disease. Data from the Organisation for Economic Co-operation and Development (OECD) and the World Health Organisation (WHO) ‘Health For All’ database on historical smoking rates have shown that, in Ireland, a convergence in smoking rates between men and women has occurred over the past 30 years. However, the impact of this convergence in smoking rates on COPD mortality and in COPD in-patient hospital morbidity has never been examined. The aim of this study was to study trends in COPD mortality and morbidity among males and females aged over 40 years in Ireland, and investigate if the convergence of smoking rates among Irish males and females was likely to have any impact on the COPD mortality and in-patient hospitalization rates.
Methods
All deaths over a ten year period 2000-2009 in those aged 40 years and over with a principle or underlying cause of death of COPD recorded were identified from the Central Statistics Office database using the following codes: ICD-9 Codes 490-492, 493.2 and 496 for years 2000-2006 inclusive and ICD-10 Codes J40-J44 and J47 for years 2007-2009 inclusive. In-patient hospital discharges for those aged 40 years and over to acute public hospital between 2000-2009 for which a principal diagnosis of COPD was recorded were extracted from the Hospital In-Patient Enquiry (HIPE). The COPD hospital discharges were identified using ICD-9 Codes 490-492, 493.2 and 496 for years 2000-2004 inclusive and using ICD 10 Codes, J40-44 and J47 for years 2005-2009. HIPE is a computer-based health information system that collects demographic, clinical and administrative data on discharges from acute public hospitals in Ireland.11 The HIPE system is managed by the Health Service Executive (HSE) and the Economic and Social Research Institute (ESRI).
To calculate COPD mortality rates, the number of deaths with COPD recorded as underlying cause of death was used as numerator and the population of Ireland was used as denominator. To calculate COPD hospital in-patient rates, the number of hospital in-patient discharges was used as numerator and the total resident population 40 years and over as the denominator. The total resident population data were extracted from the Health Atlas database that includes census and inter-censual data from the Central Statistics Office of Ireland.12 Rates were standardized to the EU standard population (direct method). Historical smoking rates were extracted from the WHO health for all database and from the OECD database. Data were analysed using JMP statistical package.13 Crude and age-adjusted rates and rate differences were calculated using StatsDirect.14 T-tests were used to compare means. Pearson’s X2 test was used to compare proportions in groups of categorical data and test for trend was used to identify linear trend and regression slopes were compared using Stata.15
Results
Number of deaths with COPD as the underlying cause of death
There were 14,519 deaths with COPD recorded as an underlying cause of death over the ten year study period (Table 1). This reduction in deaths led to a decrease in the age standardized mortality rate for men and women. However, the decrease was significantly greater for the men (test for trend, p<0.01 for men vs. p=0.06 for women). The rate difference between the male and female COPD mortality rate in 2000 was significantly larger than the rate difference in 2009 (i.e. a rate difference of 27 per 100,000 (95% CI 22.9 to 31.0) in 2000 compared to a rate difference of 14 per 100,000 (95% CI 11.6 to 17.8) in 2009. This has led to a convergence in the male and female mortality rates and as shown in Figure 1, if the rate of mortality continues the same the female mortality rate will surpass the male mortality rate in 10 years.
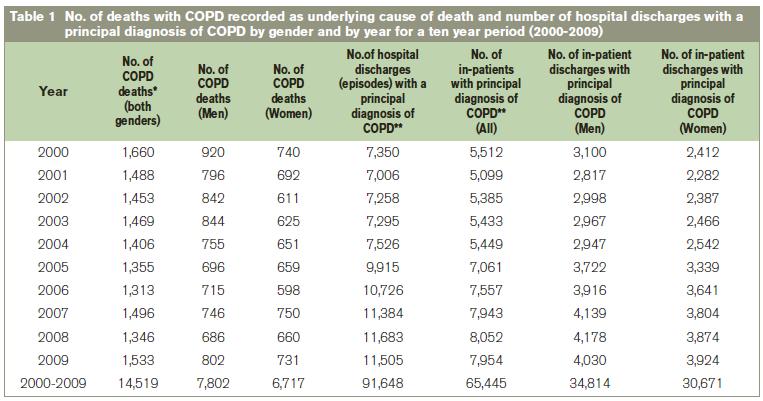
*ICD-9 Codes 490-496 excluding 493 for years 2000-2006, and ICD-10 codes J40-J47, excluding J45-J46 for 2007-2009.
**ICD-9 Codes 490-492, 493.2 and 496 for years 2000-2004 and ICD-10 Codes J40-J44 and J47 for years 2005-2009.
Number of in-patient hospital discharges with a principal diagnosis of COPD for those aged ≥40 years as recorded by year of discharge
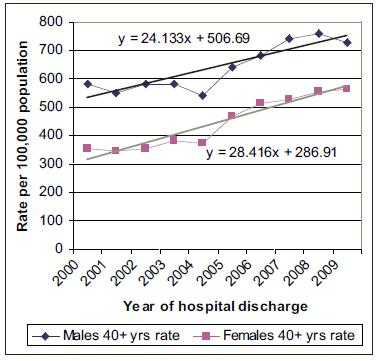
There were 91,648 hospital discharges representing 65,445 patients with a principal diagnosis of COPD over the ten year study period (Table 1). The number of discharges increased by 56.1% over the study period from 7,350 in 2000 to 11,505 in 2009. This represents an increase of 44.3% in the number of patients over the study period from 5,512 in 2000 to 7,954 in 2009. However the increase in the number of patients was significantly greater in the women compared to the men over the ten year study period (62.7% vs., 30.0%, p<0.001). As shown in Figure 2, the age standardized hospital discharge rate was greater for the women (test for trend, p<0.004 for women vs. p=0.01 for men) The rate difference between the male and female hospital discharge rate in 2000 was significantly larger than the rate difference in 2009 (i.e. a rate difference of 222.5 per 100,000 (95% CI 204.7 to 246.3) in 2000 compared to a rate difference of 165.9 per 100,000 (95% CI 139.0 to 192.8 per 100,000) in 2009. This has led to a convergence in the male and female hospital discharge rates (Figure 2).
Figure 1: Age standardized mortality rate for deaths with COPD recorded as underlying cause of death by year of occurrence.
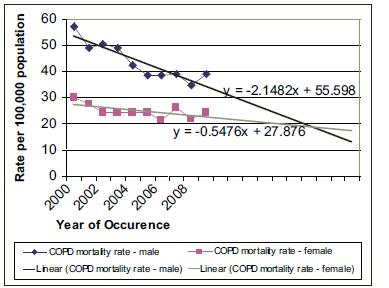
Figure 2: Age standardized hospital discharge rate for COPD by year of hospital discharge.
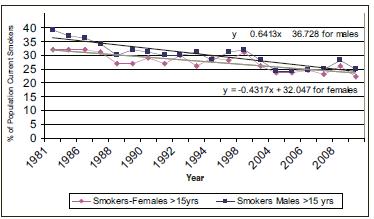
Cigarette smoking rates in Ireland over a 30 year period
The prevalence of cigarette smoking in Ireland has reduced over the past 30 years for both men and women (Figure 3). However, there was a greater significant reduction in prevalence of cigarette smoking in men i.e., 14.1% (95% CI 10.5 to 26.6, p=0.03) (i.e. from 39% in 1981 to 24.9% in 2010) compared to a non-significant reduction in smoking rate for women i.e., 9.9% (95% CI 2.3 to 22.2, p>0.05) (i.e. from 32% in 1981 to 22.1% in 2010). This has led to a convergence in smoking rates (Figure 3) that mirrors the trend in the convergence of COPD mortality and in-patient hospital discharge rates among Irish men and women.
Hospital profile of hospital discharges with a principal diagnosis of COPD
The median length of stay was 7 days (range 1-730 days) with a total of 894,325 bed days over the ten year study period. Women had a significantly longer length of stay compared to the men (10.1 days vs. 9.5 day, p<0.01). The majority were emergency admissions (71,663, 78.2%) with the majority being discharged home (77,099, 84.1%) and a significant minority (3,741, 4.1%) who died in hospital.
Profile of patients admitted with a principal diagnosis of COPD
Over the ten year study period, the majority of the patients were male (The average age of patients aged over 40 years with a principal diagnosis of COPD was 71.4 (S.D. 10.7) years. Female patients were on average, significantly younger than the men (71.1 years vs. 71.8 years, p<0.001).
Figure 3: Smoking prevalence figures for men and women aged >15 yrs by year.
Discussion
This is the first study in the Republic of Ireland to examine the effect of the convergence of historical smoking rates on COPD mortality and COPD hospital in-patient discharges. This is a cross-sectional study and although the changing smoking rates in Irish women could be a causative factor in the increase in COPD among women, this causal relationship can only be inferred and it has not been proven. Factors other than smoking may be leading to the convergence in COPD deaths and hospital discharges. However, there has also been a convergence in the incidence of lung cancer in Irish men and women and it has been hypothesized that this convergence is also due to the convergence in smoking rates between Irish men and women.16 This study was limited to data on COPD mortality and COPD in-patient hospital morbidity. Clearly there is a need for more comprehensive data on all aspects of COPD in Ireland (for e.g. ED data and GP data). There are no data available on smoking history or on severity of COPD disease and this information would have been useful to infer causality.
This study found a reduction in COPD mortality rates but an increase in COPD hospital discharge rates. However, the reduction in COPD mortality rates was significantly greater among the men compared to the women. This significant reduction in mortality in Irish men mirrors the reduction in their smoking rates. The slower rate of reduction in COPD deaths among women is likely to reflect the slower rate of decline in smoking rates among Irish women. If the trend continues, the female COPD mortality rate for women will surpass the male COPD mortality rate in ten years. This study has also shown that there has been a convergence in the in-patient hospital discharge rate for COPD in men and women in Ireland. Given that patients admitted to hospital with COPD are likely to be suffering from severe exacerbations of the disease, the finding that female patients admitted with COPD were on average younger than male patients adds more evidence to the premise that women are more likely than men to develop early-onset COPD.17
This study also highlights the substantial burden of COPD on acute hospital services in Ireland with lengthy hospital stays and repeat admissions being common. Given that our population is ageing and there is a greater number of older women than men in Ireland, we need to prepare for the growing burden of this disease on our health services by ensuring that adequate resources and best evidence based practice is used to care for these patients. Additional sustained and effective smoking cessation programmes need to be in place and targeted at women. An evidence-based approach to the management of COPD similar to that outlined in the WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD)18 should be implemented with particular emphasis on smoking cessation targeted at both men and women. Educating patients, physicians, and the public to recognize that COPD is a preventable disease that may in the future be as common among women is of great importance. Continued monitoring of trends in COPD mortality and morbidity must be carried out.
Correspondence: A O'Farrell
Health Intelligence Unit, HSE, Palmerstown, Dublin 20
Email: [email protected]
References
1. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global burden of disease and risk factors. New York: Oxford University Press; 2006.
2. Schirnhofer L, Lamprecht B, Vollmer WM Allison MJ, Studnicka M, Jensen RL, and Buist AS (2007).COPD prevalence in Salzburg, Austria: results from the Burden of Obstructive Lung Disease (BOLD) Study. Chest., 131: 29-36.
3. Sullivan SD, Ramsey SD, and Lee TA, (2000). The economic burden of COPD. Chest., 117: 5S-9S.
4. Central Statistics Office (2010). Vital Statistics 2000-2010. CSO, Dublin, Ireland.
5. Wilson D, Adams R, Appleton S. et al (2005). Difficulties identifying and targeting COPD and population-attributable risk of smoking for COPD: a population study. Chest, 2005. 128: 2035-42.
6. Burrows B, Knudson RJ, Cline MG and Lebowitz MD.(1977). Quantitative relationship between cigarette smoking and ventilatory function. Am. Rev. Respir. Dis., 1977. 115: 195-205.
7. Greaves LJ and Richardson LA (2007). Tobacco use, women, gender, and chronic obstructive pulmonary disease: are the connections being adequately made? Proc. Am. Thorac. Soc., Dec;4: 675-9.
8. Chen Y, Horne SL, and Dosman JA (1991). Increased susceptibility to lung dysfunction in female smokers. Am. Rev. Respir. Dis., Jun;143: 1224-30.
9. Prescott E, Bjerg AM, Anderson PK, Lange P and Vestbo J. (1997). Gender difference in smoking effects on lung function and risk of hospitalization for COPD: results from a Danish longitudinal population study. Eur. Respir. J., Apr;10: 822-827.
10. Sørheim IC, Johannessen A, Gulsvik A, Bakke PS, Silverman EK and DeMeo DL. (2010). Gender differences in COPD: are women more susceptible to smoking effects than men? Thorax, 65: 480-5.
11. Department of Health and Children (2002). Activity in Acute Public Hospitals in Ireland. The Economic and Social Research Institute: Dublin, Ireland.
12. Central Statistics Office. (2010). Vital statistics. Dublin, Ireland.
13. SAS Institute (2001). JMP statistical package. Cary, North Carolina, USA.
14. StatsDirect (2003). StatsDirect statistical programme. Cheshire, United Kingom.
15. SAS Institute (2002). Stata statistical package. Cary, North Carolina, USA.
16. National Cancer Research Registry Ireland. (2011). Cancer in Ireland 2011. Annual Report of the National Cancer Registry of Ireland. Cork, Ireland.
17. Dransfield M, Davis J, Gerald L and Bailey W. (2006). Racial and gender differences in susceptibility to tobacco smoke among patients with chronic obstructive pulmonary disease? Respir. Med., 100: 1110-1116.
18. World Health Organisation (2001). Global Initiative for Chronic Obstructive Lung Disease (GOLD). Geneva, Switzerland.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|