|
|
|
|
|
|
|
|
Fiachra Moloney,Desiree Fernandez,hugh harrington
|
|
|
Ir Med J. 2012 Mar;105(3):84-5
F Moloney, D Fernandez, H Harrington
Cork University Hospital, Wilton, Cork
Abstract
Progressive multifocal leucoencephalopathy (PML) is an opportunistic, demyelinating neurological disease caused by reactivation of the JC polyomavirus. PML occurs almost exclusively in immunosuppressed individuals, with only isolated case reports of PML occurring in patients without apparent immunosuppression. Idiopathic CD4+ lymohocytopenia (ICL) is a syndrome defined by the Centre for Disease Control and Prevention as a CD4+ count < 300 cells/uL or <20% of total T cell count on > 1 occasion, with no evidence of human immunodeficiency virus (HIV) infection, and the absence of other known immunodeficiency or therapy associated with lymphocytopenia. We describe a case of PML occurring in a patient with idiopathic CD4+ lymphocytopenia.
|
Introduction
Progressive multifocal leucoencephalopathy (PML) is an opportunistic, demyelinating neurological disease caused by reactivation of the JC polyomavirus. PML occurs almost exclusively in immunosuppressed individuals, with only isolated case reports of PML occurring in patients without apparent immunosuppression. PML is recognised as a major opportunistic infection in acquired immunodeficiency syndrome (AIDS) with a prevalence of 1 to 5 percent1. PML has been described in patients with haematological malignancies, transplant recipients and those receiving immunosuppressive agents. Idiopathic CD4+ lymohocytopenia (ICL) is a syndrome defined by the Centre for Disease Control and Prevention as a CD4+ count < 300 cells/uL or <20% of total T cell count on > 1 occasion, with no evidence of human immunodeficiency virus (HIV) infection, and the absence of other known immunodeficiency or therapy associated with lymphocytopenia2. The aetiology of ICL is currently unknown. Clinical presentations range from an isolated laboratory finding to life-threatening opportunistic infections. We describe a case of PML occurring in a patient with idiopathic CD4+ lymphocytopenia.
Case Report
A 55 -year-old right handed man presented with gradual onset left upper limb weakness. This progressed over a period of 3 months to a dense left hemiparesis. His past medical history was unremarkable and he had no risk factors for HIV infection. On admission the patient was afebrile, normotensive (blood pressure 124/66mmHg) and in sinus rhythm (heart rate 69 beats/min). Neurological examination revealed a left upper motor neurone facial palsy with weakness of the left arm and leg associated with brisk deep tendon reflexes. This patient also had speech dysarthria and fasciculations of the deltoid and triceps muscles bilaterally. Physical examination was otherwise unremarkable. There was no decline in cognitive function.
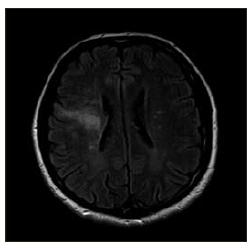
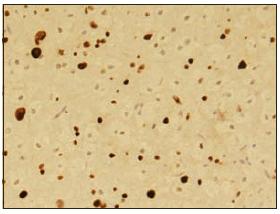
MRI brain demonstrated an ill-defined area of non-enhancing high signal intensity in the right hemisphere, extending from the pericallosal fibres superiorly to the subcortical grey and white matter (Figure 1). Histological examination of a stereotactic biopsy sample revealed focal demyelination associated with reactive astrocytosis and hugely enlarged and smudged oligodendrocyte nuclei. The presence of JC virus infected oligodendrocytes was confirmed by immunohistochemistry (Figure 2). A full blood count revealed lymphocytopenia with a lymphocyte count of 0.77 (1-4x109/L). The CD4+ lymphocyte count was 5% of total lymphocytes with an absolute count of 39. A repeat CD4+ count at two weeks was 6% of the total lymphocytes with an absolute count of 33. Serological tests for antibobies to HIV-1 and HIV-2 were negative, as was PCR for HIV DNA.
Figure 1. Magnetic resonance image (T2 flair) of the brain of a patient with progressive multifocal leucoencephalopathy. There is an ill-defined area of increased signal intensity in the right hemisphere without enhancement on the T1 weighted post gadolinium images.
Cerebrospinal fluid (CSF) analysis showed 3 lymphocytes/mm3; glucose 4.2 mmol/L (>50% of plasma glucose) and protein 1.16 g/L. CSF PCR for opportunistic infections including cytomegalovirus, herpes simplex virus, varicella-zoster virus and Epstein-Barr virus was negative. Bone marrow aspiration revealed normal cellularity. CT thorax, abdomen and pelvis excluded underlying malignant neoplasm. Syphilis serology was negative. Immunoglobulins, autoimmune screen (antinuclear antibodies, antineutrophil cytoplasmic antibody, anti-extractable nuclear antigen, rheumatoid factor, anti-double-stranded DNA antibody, anti-La and anti-Ro antibodies) and complement levels were normal.
Figure 2: Histological findings of the stereotactic biopsy of a patient with PML; immunohistochemistry showing positive brown signal in the nuclei of virus infected oligodendrocytes.
Discussion
PML is most commonly associated with HIV infection. Highly active antiretroviral therapy (HAART) has been shown to prolong survival in PML associated with HIV infection.3 Little data exists regarding PML treatment in HIV negative patients. Cidofovir has been used in patients with PML and HIV, but the largest clinical trial reports no benefit.4 Similarly, cidofovir therapy had no benefit in patients with PML and ICL.5,6 Mirtazepine may offer benefit to HIV negative patients with PML but evidence for this is provided only by isolated case reports.7,8 Intravenous cytarabine has been shown to benefit HIV negative patients with PML and haematological malignancy in one open label study.9 However, in a randomised control trial of PML patients with HIV, cytarabine did not improve prognosis.10 Only five cases of PML occurring in patients with ICL have been described in the literature to date.5 This case highlights the lack of treatment for PML occurring in all disease states and the lack of understanding of the ICL syndrome.
Correspondence: F Moloney
Tearmann, barntick, Clarecastle, Ennis, Co Clare
Email: [email protected]
References
1. Holman RC, Janssen RS, Buehler JW, Zelasky MT, Hooper WC. Epidemiology of progressive multifocal leucoencephalopathy in the United States: analysis of national mortality and AIDS surveillance data. Neurology. 1991 Nov; 41:1733-6.
2. Smith DK, Neal JJ, Holmberg SD. Unexplained opportunistic infections and CD4+ T-lymphocytopenia without HIV infection. An investigation of cases in the United States. The Centres for Disease Control Idiopathic CD4+ T-lymphocytopenia Task Force. N Engl J Med. 1993; 328:373.
3. Kaplan JE, Benson C, Holmes KH, PAU A, Masur. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and children: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009; 58:1.
4. De Luca A, Ammassari A, Pezzotti P Cinque P, Gasnault J. Cidofovir in addition to antiretroviral treatment is not effective for AIDS-associated progressive multifocal leukoencephalopathy: a multicohort analysis. AIDS. 2008; 22:1759-1762.
5. Melzi S, Bonfanti P, Carenzi L Faggion I, Resta M, Resta F, Rizzardini G. Progressive multifocal leucoencephalopathy in a patient with idiopathic CD4+ cells deficit. Clin Ter. 2008; 159:325-7.
6. Haider S, Nafziger D, Gutierrez J, Brar I, Mateo N, Fogle J.Progressive multifocal leucoencephalopathy and idiopathic CD4+ lymphocytopenia: a case report and review of reported cases. Clin Infec Dis. 2000; 31:20-2.
7. Verma S, Cikurel K, Koralnik I, J Morgello S, Cuningham C, Weinstein Z, Bergmann C, simpson DM. Mirtazapine in progressive multifocal leukoencephalopathy associated with polycythemia vera. J Infect Dis. 2007; 196:709.
8. Vulliemoz S, Lurati-Ruiz F, Borruat FX Ruiz F, Borruat F, Dellavelle J. Favourable outcome of progressive multifocal leucoencephalopathy in two patients with dermatomyositis. J Neurol Neurosurg Psychiatry. 2006; 77:1079.
9. Aksamit AJ. Treatment of non-AIDS progressive multifocal leukoencephalopathy with cytosine arabinoside. J Neurovirol. 2001; 7:386.
10. Hall CD, Dafni U, Simpson D Clifford D, Wetherill PE, Cohen B, McArthur J, Hollander H, Major E, Miller L, Timpone J. Failure of cytarabine in progressive multifocal leukoencephalopathy associated with human immunodeficiency virus infection. AIDS Clinical Trials Group 243 Team. N Engl J Med. 1998; 338:1345.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|