|
|
|
|
|
|
|
|
RC Tarrant,M Sheridan-Pereira,KM Younger,JM Kearney
|
|
|
|
Ir Med J. 2012 Mar;105(3):75-8
|
|
RC Tarrant1, M Sheridan-Pereira1,2, KM Younger3, JM Kearney3
1Our Lady’s Children’s Hospital, Crumlin, Dublin 12
2Coombe Women & Infants University Hospital, Cork Street, Dublin 8
3Department of Biological Sciences, Dublin Institute of Technology, Dublin 8
Abstract
This study aimed to report on adverse infant and maternal clinical outcomes, and investigate the relationship between infant feeding practice and such adverse clinical outcomes in infants during the first 6 weeks postpartum. From an eligible sample of 450 mother-term infant pairs recruited from the Coombe Women and Infants University Hospital in Dublin, 27.1% of infants (n=122) were maternally reported to have had an illness during the first 6 weeks that necessitated the provision of prescribed medication ± general practitioner/paediatrician attendance ± hospitalisation. Of these, 90 infants had ≥ 1 episode of infection ± viral ± gastro-intestinal-related condition. After adjustment, ‘any’ breastfeeding to 6 weeks was protective against such adverse infant outcomes (adjusted odds ratio [aOR] 0.44, P = 0.022). Attendance to the GP/paediatrician for > 1 visit (aOR 3.44, P = 0.000) and multiparity (aOR 1.76, P = 0.041) were also positively associated with such adverse infant outcomes. To decrease infant morbidity rates in Ireland, government investment in breastfeeding promotion, support and research should be a continued public health priority.
Introduction
To ensure optimal infant and maternal health outcomes, the World Health Organisation (WHO)1 recommends exclusive breastfeeding during the first 6 months of life; a guideline that was adopted by the Irish Department of Health and Children in 2003. Although exclusivity of the practice up to 6 months is a desirable goal, partial breastfeeding as well as breastfeeding for shorter periods of time are also valuable2. The evidence for the protective effects of breastfeeding against infant risk of acute otitis media3, gastro-intestinal4 and respiratory5,6 morbidity, is particularly convincing2. According to the UK Millennium Cohort Study, an estimated 53% of hospitalisations due to infant diarrhoea could be prevented each month by exclusive breastfeeding and 31% by partial breastfeeding7. A meta-analysis by Bachrach et al.8 showed a 72% reduction in the risk of hospitalisation due to respiratory diseases in exclusively breastfed (to ≥ 4 months) compared with formula fed term infants in developed settings.
A population-level increase in exclusive and prolonged breastfeeding would be of considerable potential public health benefit for Ireland. However, Irish breastfeeding rates have historically been, and currently remain, among the lowest worldwide9,10. Although robust evidence from international studies associate a history of breastfeeding with optimal infant health, to date, no published Irish study has examined the effect of infant feeding practice on adverse clinical outcomes in infants. The present study sought to report on adverse infant and maternal clinical outcomes, and investigate the relationship between type of infant feeding practice and such adverse clinical outcomes in an Irish cohort of term infants during the first 6 weeks postpartum.
Methods
Detailed methods and sample representativeness of this prospective observational study are already described in detail11. In summary, from an initial sample of 539 low risk pregnant women recruited from antenatal clinics in the Coombe Women and Infants University Hospital (CWIUH), Dublin, 450 eligible mother-term infant pairs were followed up via face-to-face or telephone interviewer-administered survey at 6 weeks (June 2004-October 2006). Infants who had a congenital abnormality, those who required medical intervention and/or tube feeding, as well as mothers who required medical intervention postpartum were all excluded from this study.
Data on whether an infant or maternal illness was experienced at any stage during the first 6 weeks were elicited from maternal self-reports, and were not verified by medical record review. Both infant and maternal illness was defined as ‘any illness that necessitated the provision of prescribed medication ± general practitioner (GP)/paediatrician attendance ± hospitalisation during the first 6 weeks’. Mothers were specifically asked to only detail the illnesses applicable to this definition. Information on the number and type of infant and maternal illness episodes was documented. Mothers were also asked to specify the number of GP/paediatrician attendances regarding their infants during the first 6 weeks. Healthy infants and mothers were those in whom no illness episodes were reported. As relatively few mothers exclusively breastfed during the first 6 months in this study11, ‘any’ breastfeeding, defined as those who provided any breast milk to their infants (expressed or via skin-to-skin contact), either exclusively (solely breast milk), or in combination with formula milk ± water, was the breastfeeding category selected for analysis.
Statistics were computed by using Statistical Package for the Social Sciences (SPSS Inc.; Chicago, USA, version 19). Data are presented using numerical descriptive statistics, including percentages for categorical data, and means with standard deviations (SD) or medians with interquartile ranges (IQR) for continuous data, as appropriate. Comparison between groups was performed using the Student’s t-test, Mann-Whitney U test or one-way between-groups ANOVA for continuous variables; the Chi-square test was employed for categorical variables. Significance was set at P<0.05. Binary logistic regression analysis was used to explore the factors associated with the dependent variable risk of ≥ 1 episode of infection ± viral-related ± gastro-intestinal-related condition in infants during the first 6 weeks. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) were calculated for each factor in the final model. The Ethics Boards of the CWIUH and the Dublin Institute of Technology approved this study.
Results
Sample characteristics
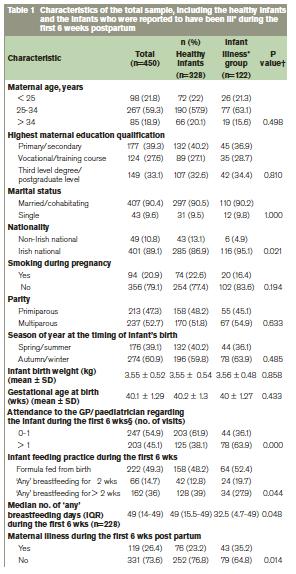
The median age of infants at the 6 week follow-up was 6.57 weeks (IQR 6.1-7). Almost half of the sample of infants (n=222; 49.3%) were formula fed from birth (Table 1). Although breastfeeding was initiated by 228 mothers (50.6%), only 162 mothers (36%) were providing ‘any’ breast milk to their infants for > 2 weeks postpartum11. Infants who were reported to have had ≥ 1 illness that necessitated the provision of prescribed medication ± GP/paediatrician attendance ± hospitalisation (n=122; 27.1%) compared with the healthy group (n=328) were significantly more likely to have: been formula fed from birth (52.4% vs 48.2%; P = 0.044), attended the GP/paediatrician for > 1 visit (63.9% vs 38.1%; P = 0.000) and to have had mothers who were also ill during the first 6 weeks (35.2% vs 23.2%; P = 0.014).
Adverse infant and maternal clinical outcomes during the first 6 weeks
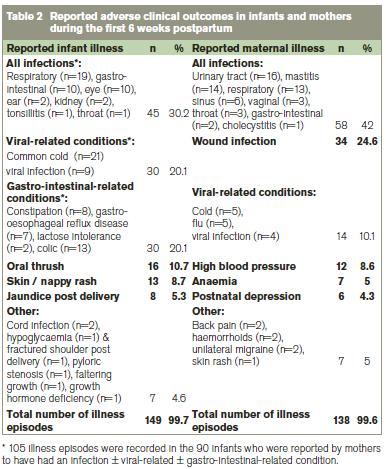
A total of 149 illness episodes were recorded in the 122/450 infants who were reported by mothers to have had an illness during the first 6 weeks (Table 2). The common cold (n=21, 14%), respiratory infection (n=19, 13%) and oral thrush (n=16, 10.7%) were the most frequently reported infant illnesses. In all, 138 illness episodes were recorded in the 119/450 mothers (26.4%) who reported having an illness during the first 6 weeks, with the most frequently reported illnesses including wound infection (n=34; 24.6%), urinary tract infection (n=16; 11.5%) and mastitis (n=14; 10.1%).
Independent effect of infant feeding practice on reported adverse clinical outcomes in infants
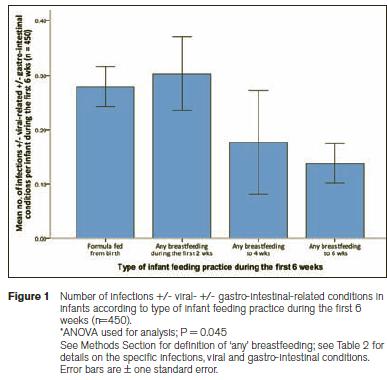
As illustrated in Figure 1, the mean number of infections ± viral ± gastro-intestinal-related conditions for the formula fed infants was significantly higher than for those breastfed to 6 weeks (mean 0.27, SD 0.54 vs mean 0.13, SD 0.43; P = 0.045). Binary logistic regression analysis indicated that infants who were provided with ‘any’ breast milk to 6 weeks (compared with the formula feeders from birth) were significantly less likely to have had ≥ 1 reported episode of infection ± viral-related ± gastro-intestinal-related condition during the first 6 weeks (aOR 0.44; 95% CI 0.22-0.88, P = 0.022) (Table 3). Infants reported to have had ≥ 1 episode of infection ± viral-related ± gastro-intestinal-related condition were 3.4 times more likely to have been brought to the GP/paediatrician for > 1 visit (compared with 0-1 visit) during the first 6 weeks (aOR 3.44; 95% CI 2.04-5.79, P = 0.000) and were almost twice as likely to have had multiparous mothers (aOR: 1.76; 95% CI 1.02-3.06, P = 0.041).

Discussion
Consistent with international data1-8, this study highlights the positive role of breastfeeding on infant health. Even after adjustment for potential confounding variables including season of year at the timing of infant’s birth, parity, maternal illness during the first 6 weeks as well as education (proxy for socio-economic status), age and smoking status during pregnancy, infants who were provided with ‘any’ breast milk to 6 weeks were significantly less likely to have had ≥ 1 reported episode of infection ± viral-related ± gastro-intestinal-related condition (aOR 0.44; 95% CI: 0.22-0.88, P = 0.022). Although the period of postpartum follow-up was relatively short in this study, notably, 6 weeks, we found that duration of breastfeeding impacted on the degree of protection against ≥ 1 episode of infection ± viral-related ± gastro-intestinal-related condition in infants, with ‘any’ breastfeeding to 6, rather than 2 or 4 weeks, exhibiting a significant benefit (P = 0.045). The trend towards increased protection of breastfeeding according to duration is also reported in robust prospective studies from Spain12, Germany13, USA3 and UK7,14.
It is of further interest from this study that infants born to Irish, compared with non-Irish national mothers were significantly more likely to have had a reported illness during the first 6 weeks (95.1% versus 4.9%, P = 0.021). The significantly lower rate of breastfeeding initiation as well as ‘any’ and exclusive breastfeeding, in the Irish, compared with the non-Irish national mothers throughout the first 6 weeks11 may be one possible explanation for this infant health disparity. Moreover, the present study found that infants in the illness versus the healthy group were provided with any breast milk for a significantly shorter duration during the first 6 weeks (32.5 days versus 49 days, P = 0.048). Although causal relationships between infant health and feeding practice cannot be concluded from this study, more rigorous evaluation of the degree to which well-defined indicators of infant health outcomes are influenced by both nationality and precise infant feeding practice parameters (e.g. frequency of daily breast milk feeds, inclusion of clear breastfeeding definitions) should be considered in future studies.
While exclusive breastfeeding up to 6 months is a desirable goal2, mothers should be informed that providing ‘any’ breast milk to their infants for short durations to even ≥ 3 months postpartum as reported by Howie et al.,14 offers a clear advantage to their infants by reducing, in particular, gastro-intestinal and respiratory infection. This is of further clinical and public health importance given that chest/respiratory infection is one of the most frequently reported adverse clinical outcomes among infants in Ireland15, and internationally8, as supported by our study. Taken together, findings from the present study should not undermine the WHO1 recommendation to exclusively breastfeeding until 6 months. Many mothers in Ireland discontinue breastfeeding early due to the frequent feeding routine, tiredness and the perception of an inadequate milk supply11,15,16. However, existing data suggest that in such circumstances there would be advantages in continuing to provide ‘any’ breast milk to their infants for even a short duration. Given that the vast majority of women are capable of breastfeeding17, all health professionals who engage with lactating mothers should inform them that ‘any’ breast milk is better than no breast milk, and that it is worthwhile persevering with the practice if they encounter problems during the initial few days, or weeks postpartum.
Multiparity was also significantly associated with risk of ≥ 1 reported episode of infection ± viral-related ± gastro-intestinal-related condition in this study (aOR 1.76; 95% CI: 1.02-3.06, P = 0.041); other investigators have reported similar findings18. It is suggested that infants with older siblings are exposed to more infectious organisms than are first-born children and that this exposure may override the protective effect of breastfeeding on the infant’s immune system18,19. Nonetheless, despite the significant association between multiparity and risk of adverse infant outcomes in this study, the protective effect of ‘any’ breastfeeding to 6 weeks still persisted in the adjusted model. To date, no previous Irish prospective study has examined the effect of infant feeding practice, GP/paediatrician attendance regarding the infant on adverse clinical outcomes, taking socio-economic factors into account. Although the design of this study does not provide definitive evidence for a protective effect of breastfeeding, or proving causality, these findings in addition to a wealth of data from existing studies, provide further evidence that breastfeeding, for even a short duration, is a worthwhile practice. As a breastfeeding promotional measure for Ireland, the inclusion of these data in literature, campaigns and strategies aimed at increasing initiation rates and duration should be considered.
Study limitations include lack of objective verification of reported infant and maternal illnesses (including their severity and duration) during the first 6 weeks. Furthermore, our follow-up data relied exclusively on maternal self-reports and re-call. However, maternal19 or parental7,13 self-reports are the primary data resource of adverse infant health outcomes in other similarly designed prospective studies. The prospective nature of the study design, high follow-up rate of mother-term infant pairs to 6 weeks, and completeness of data are some of the strengths of this study. In addition, information collected on type of infant feeding practice was comprehensive. In conclusion, our findings demonstrate the positive role of breastfeeding on infant health during the first 6 weeks postpartum. To ensure optimal health for all infants, these data lend support to the clinical and public health importance of investing in the promotion of breastfeeding in Ireland. Mothers should be informed that although exclusive breastfeeding up to 6 months is a desirable goal, the provision of ‘any’ breast milk to their infants for even a short duration, also confers considerable health benefit.
Acknowledgements
The authors are extremely grateful to the study participants. We are also indebted to the clinical and administrative staff in the Coombe Women and Infants University Hospital for their practical help and support throughout the study. A special thank you is extended to Roberta McCarthy for her help with manuscript revision.
Correspondence: RC Tarrant
Department of Clinical Nutrition and Dietetics, Our Lady’s Children’s Hospital, Crumlin, Dublin 12
Email: [email protected]
References
1. World Health Organisation 54th World Health Assembly 2001. Global strategy for infant and young child feeding: the optimal duration of exclusive breast feeding. Geneva, WHO: Department of Child and Adolescent Health and Development.
2. ESPGHAN Committee on Nutrition, Agostoni C, Braegger C, Decsi T, Kolacek S, Koletzko B, Michaelsen KF, Mihatsch W, Moreno LA, Puntis J, Shamir R, Szajewska H, Turck D, van Goudoever J. Breast-feeding: A Commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr 2009; 49: 112-25.
3. Duncan B, Ey J, Holberg CJ, Wright AL, Martinez FD, Taussig LM Exclusive breast-feeding for at least 4 months protects against otitis media. Pediatrics 1993; 91: 867-72.
4. Chien PF, Howie PW. Breast milk and the risk of opportunistic infection in infancy in industrialized and non-industrialized settings. Adv Nutr Res 2001; 10: 69-104.
5. Silvers KM, Frampton CM, Wickens K, Epton MJ, Pattemore PK, Ingham T, Fishwick D, Crane J, Town GI; New Zealand Asthma and Allergy Cohort Study Group. Breastfeeding protects against adverse respiratory outcomes at 15 months of age. Matern Child Nutr 2009; 5: 243-50.
6. Duijts L, Jaddoe VW, Hofman A, Moll HA. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics 2010; 126: e18-25.
7. Quigley MA, Kelly YJ, Sacker A. Breastfeeding and hospitalization for diarrheal and respiratory infection in the United Kingdom Millennium Cohort Study. Pediatrics 2007; 119: e837-42.
8. Bachrach VR, Schwarz E, Bachrach LR. Breastfeeding and the risk of hospitalization for respiratory disease in infancy: a meta-analysis. Arch Pediatr Adolesc Med 2003; 157: 237-43.
9. Tarrant RC, Kearney JM. Session 1: Public health nutrition. Breast-feeding practices in Ireland. Proc Nutr Soc 2008; 67: 371-80.
10. Organisation for Economic Co-operation and Development (OECD) Database on Breastfeeding Rates (CO1.5) 2009. doi: http://www.oecd.org/dataoecd/30/56/43136964.pdf (accessed February 2012).
11. Tarrant RC, Younger KM, Sheridan-Pereira M, White MJ, Kearney JM. The prevalence and determinants of breast-feeding initiation and duration in a sample of women in Ireland. Public Health Nutr 2010; 13: 760-70.
12. Paricio Talayero JM, Lizán-García M, Otero Puime A, Benlloch Muncharaz MJ, Beseler Soto B, Sánchez-Palomares M, Santos Serrano L, Rivera LL. Full breastfeeding and hospitalization as a result of infections in the first year of life. Pediatrics 2006; 118: e92-9.
13. Rebhan B, Kohlhuber M, Schwegler U, Fromme H, Abou-Dakn M, Koletzko BV. Breastfeeding duration and exclusivity associated with infants' health and growth: data from a prospective cohort study in Bavaria, Germany. Acta Paediatr 2009; 98: 974-80.
14. Howie PW, Forsyth JS, Ogston SA, Clark A, Florey CD. Protective effect of breastfeeding against infection. BMJ 1990; 300: 11-6.
15. Williams J, Greene S, McNally S, Murray A, Quail A. Growing Up in Ireland: the infants and their families infant cohort 2010. Dublin: The Stationery Office. doi: http://www.growingup.ie/fileadmin/user_upload/Conference_2010/Growing_Up_in_Ireland_-_The_Infants_and_their_Families.pdf (accessed February 2012).
16. Begley C, Gallagher L, Clarke M, Carroll M, Millar S. The National Infant Feeding Survey 2008. Dublin, Ireland: The Health Service Executive. http://www.breastfeeding.ie/uploads/files/National_Infant_Feeding_Survey_2008.pdf (accessed February 2012).
17. World Health Organisation, Health 21- health for all in the 21st Century 1999. Denmark, World Health Organisation Regional Office for Europe.
18. Raisler J, Alexander C, O’Campo P. Breast-feeding and infant illness: a dose-response relationship? Am J Public Health 1999; 89: 25-30.
19. Pettigrew MM, Khodaee M, Gillespie B, Schwartz K, Bobo JK, Foxman B. Duration of breastfeeding, daycare, and physician visits among infants 6 months and younger. Ann Epidemiol 2003; 13: 431-5.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|