|
|
|
|
|
|
|
|
J Martin,J Barry,M Skally
|
|
|
|
Ir Med J. 2011 May;104(5):140-4
|
|
J Martin1, J Barry2, M Skally3
1Department of Health and Children, Hawkins House, Dublin 2
2Department of Public Health and Primary Care, Trinity College, Dublin 2
3National Cancer Registry, Cork Airport Business Park, Kinsale Road, Cork
Abstract
The aim of this study was to calculate the number and costs of hospital bed-days due to alcohol use in Ireland over the five year period 2000 to 2004. Age and sex specific Irish alcohol-attributable-fractions (AAFs) were developed by combining international risk estimates with Irish consumption data where available; where not available international AAFs were used. These were applied to national datasets to count the number and costs of bed-days wholly caused and prevented by alcohol and that proportion of bed-days that were partially caused and prevented by alcohol. Between 2000 and 2004, alcohol was estimated to have caused 3,428,973 (10.3%) and prevented 529,239 (1.6%) of hospital bed-days, giving a net number of bed-days due to alcohol of 2,899,734 (8.7%). Over this period the hospital inpatient costs attributed to the negative effects of alcohol were €953,126,381, the costs attributed to hospitalisations prevented were €147,968,164; giving net costs of alcohol-attributed bed-days of €805,158,217. Chronic conditions accounted for 3,262,408 (95%) hospital bed-days due to the harmful effects of alcohol. Conditions not wholly due to alcohol accounted for 2,297,412 (67%) hospital bed-days due to the harmful effects of alcohol. The negative impacts of alcohol were greater than previously thought and spread across the whole population.
Introduction
It is known that alcohol is widely used throughout Irish society. Irish adults aged 15 years and over are the fourth highest per capita consumers of pure alcohol in the world1. In Ireland up until now, the focus of alcohol research has been on those people dependent on alcohol, and those conditions, which are wholly or very largely attributed to alcohol2. However the prevention paradox which states “a large number of people at a small risk may give rise to more cases of disease than the small number who are at a high risk”3, would suggest that alcohol-related problems in a population come more from moderate drinkers than from heavy drinkers4. The most internationally validated method used to investigate alcohol related problems in a population is the alcohol attributable fraction (AAF). The AAF calculates the proportion of cases recorded in a population with a particular condition that is estimated to be caused or prevented by alcohol. It is that proportion of the condition that would be reduced if alcohol consumption was eliminated5. The AAF varies from country to country as a consequence of a number of factors such as differences in the levels and patterns of drinking6. The distinguishing characteristic of AAF methods is that individual alcohol caused or prevented cases are not identified7.
Recent studies have shown that in Western Europe alcohol consumption and attributable burden of disease is high compared to global averages8. In Ireland the quantity and pattern of consumption is known to be particularly problematic2,9. Mongan et al, established that alcohol accounted for at least 2.9% of all bed-days in Ireland10. However, there have not been studies to date that accurately reflect the hospitalisations due to alcohol and their associated costs across all injury and disease categories known to be causally related to alcohol. The study aim was to use the AAF method to calculate the burden of alcohol on the Irish hospital system in terms of bed-days and financial costs.
Methods
The key process was the calculation of an Irish specific AAF that could be applied to Irish datasets to quantify the number of hospital bed-days caused and prevented by alcohol and the costs associated with this. Where appropriate the indirect AAF was used. This involved two pieces of information: (1) relative risk of the association between alcohol consumption and disease or injury and (2) alcohol consumption by sex and five year age groups. Relative risks for the association, either positive (alcohol increases risk of outcome) or negative (alcohol decreases risk of outcome), between injury/disease and differing levels of alcohol consumption, and by age and sex where available, were identified from meta-analyses in the international literature. Relative risk estimates were extracted from the work undertaken by Rehm et al8, with the exception of colorectal cancer, where the relative risk came from Cho et al11, and ischemic heart disease (IHD), where the relative risk came from Ridolfo and Stevenson12. A discussion in relation to the literature used to determine relative risk is described in detail elsewhere13.
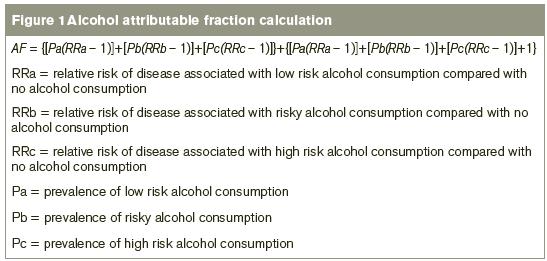
Irish alcohol consumption was calculated by combining survey data and alcohol sales data. Adult per capita consumption derived from the Revenue Commissioner’s alcohol sales data and the Central Statistics Office (CSO) population data for 2006 was taken to be the best indicator of overall consumption in Ireland. Data from the national Survey of Lifestyles, Attitudes and Nutrition 2007 (SLÁN 2007, a nationally representative sample of 10,364 respondents who completed a health interview which included an assessment of alcohol consumption patterns)9 was used to quantify sex- and age-specific abstinence and alcohol consumption patterns. Average reported daily volume of consumption for each person was increased by a factor of three to adjust for the factor by which it underestimated the per capita quantity in order to calculate the proportion of males and females, who were abstainers, low, risky and high-risk alcohol consumers. The majority of indirectly calculated AAFs were based on the sum of the partial AAFs (Figure 1).
Where it is not possible to use the indirect method e.g. for injuries, AAF’s are derived directly based on observations of the number of outcomes due to levels of alcohol considered to have caused that outcome and are based on large case series. No suitable case series in the Irish population were available and therefore the international AAFs derived by Ridolfo and Stevenson were used12. Health Atlas Ireland14 was used to access the Hospital In-Patient Enquiry Scheme (HIPE), which collects data from 62 acute public hospitals in Ireland15 and extract the number of hospital bed-days in each of the alcohol related categories and the Diagnostic Related Group (DRG) costs for those categories. The National Psychiatric In-patient Reporting System (NPIRS)16 was used to extract the number of hospital bed-days in each of the alcohol related categories presenting to psychiatric hospitals. In the absence of an equivalent costing system for NPIRS data, the DRG costs for acute hospitals were applied to bed-days for psychiatric hospitals. AAFs were applied to these datasets to quantify the number and costs of bed-days caused and prevented by alcohol use in Ireland from 2000 to 2004.
Results
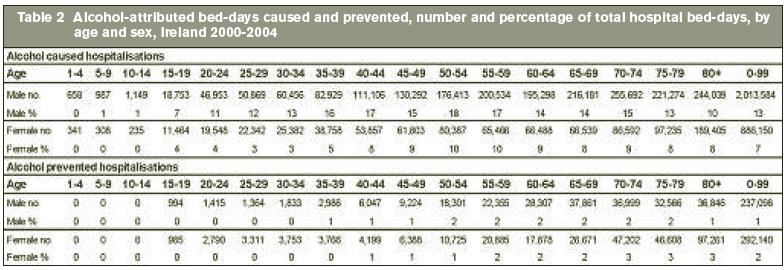
The number and proportion of bed-days caused or prevented by alcohol, by sex and condition are presented in Table 1. Over the five year period 2000-2004 10.3% (3,428,973) of bed-days were due to the harmful effects of alcohol. In this period 1.6% (529,239) of bed-days were prevented by the beneficial effects of alcohol, leading to a net 8.7% (2,899,734) of total hospital bed-days due to alcohol. In all cases the impact of alcohol on hospital bed-days was greater in men than women and greater in young to middle aged people than older people (Table 2). In men, an estimated 1% of bed-days were prevented by alcohol, while in women an estimated 2% of bed-days were prevented by alcohol. In young people there were no bed-days prevented by alcohol (Table 2). Sixty-nine percent of all hospitalisations due to alcohol were seen in women over 70 years of age. Thirty-seven percent of male bed-days due to alcohol were due to conditions wholly attributed to alcohol, whereas in females the proportion was 25%, with the remaining bed-days caused by conditions partially attributable to alcohol.
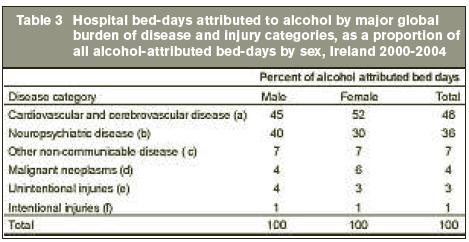
Four percent of bed-days attributed to the harmful effects of alcohol were due to the acute conditions associated with alcohol, and 96% were due to chronic conditions associated with alcohol. Cardiovascular and cerebrovascular diseases accounted for 48% of bed-days due to alcohol with neuropsychiatric disease accounting for 36% (Table 3). Over the five year period, the cost of bed-days attributable to the negative effects of alcohol was €953,126,381; the cost of bed-days prevented by alcohol was €147,968,164, resulting in a net cost of alcohol-attributable bed-days of €805,158,217, which represented 15% of total hospital costs for the time period. For men, the net costs attributable to alcohol were more than twice that of their female counterparts (€547,904,448 in men compared with €257,253,769 in women).
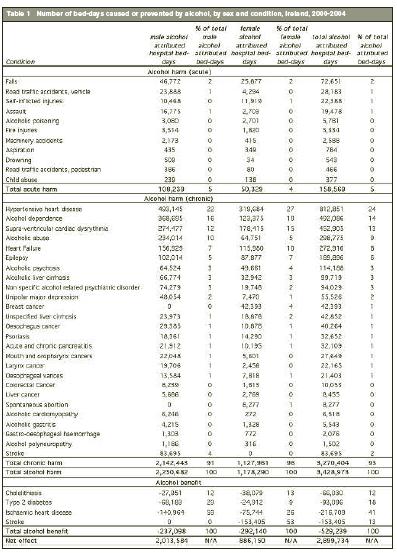
*Diseases for which alcohol had a protective effect were not included in calculation of bed-days due to alcohol
(a) Stroke, hypertensive heart disease, supra-ventricular cardiac dysrhythmia, alcoholic cardiomyopathy, heart failure
(b) Alcohol dependence, alcohol abuse, alcohol psychosis, unipolar major depression, epilepsy, alcoholic polyneuropathy, unspecified alcoholic psychiatric disorder
(c) Alcoholic and unspecified liver cirrhosis, gastro-oesophageal haemorrhage, acute and chronic pancreatitis, oesophageal varices, type 2 diabetes, alcoholic gastritis
(d) Cancers of the mouth, oropharynx, liver, larynx, breast, colorectum
(e) Road traffic accidents, falls, fire injuries, drowning, machinery accidents, aspiration, alcoholic poisoning, elevated blood alcohol level
(f) Self-inflicted injuries, assaults, child abuse
Discussion
To date, Irish research on the outcomes due to alcohol has focussed on either high risk alcohol consumers or on outcomes either wholly or mostly attributable to alcohol3. This study showed for the first time the full burden of alcohol on the Irish hospital system by using the AAF methodology to quantify the impact of alcohol across the spectrum of alcohol consumption (not only the impact on those dependent on alcohol or those who drink to intoxication) and the full range of injuries/diseases causally associated with alcohol (rather than only diseases for which alcohol is the main or sole cause).
Our study supports previous findings that the negative effects of alcohol are much greater in men than in women and that young people are disproportionately affected by the negative consequences of alcohol8,10,17-20. However, we found that the number of bed-days attributed to alcohol were many times higher than those calculated previously in Ireland. This difference was not surprising as previous research only counted bed-days wholly attributable to alcohol10, which we have shown to account for only 33% of all alcohol attributable bed-days. Chronic conditions accounted for the vast majority of alcohol attributed hospitalisations in all age groups, except children less than 15 years. Cardiovascular followed by neuropsychiatric disease was responsible for the majority of hospital bed-days with neoplasms, injuries and other non-communicable diseases comprising a smaller portion. In younger age groups acute conditions were a more common cause of hospital bed-days compared with older people, even in younger people, chronic conditions were seen to be responsible for the majority of hospital bed-days.
The protective effect of low alcohol consumption levels, mainly evident in preventing cardiovascular disease, against hospitalisations was seen only in older age groups of both sexes. This however was of a lesser magnitude than seen in other developed countries19,21-23. Reasons for this may include the fact that the Irish population is younger than other developed countries24. It is also likely to be due to the Irish pattern of drinking, with a high overall volume of consumption and episodes of ‘binge’ drinking, which is known not only to provide no protection against cardiovascular and other diseases where alcohol at low levels can have a protective effect, but to increase risk of those diseases25. Alcohol-attributed hospital bed-days accounted for €953,126, 381 of hospital costs over the five year period. Patients attending GPs, outpatient services, emergency departments and private hospitals were not included in any of the databases and therefore these costs represent only a portion of total hospital costs and a small portion of total healthcare costs. However, even this conservative estimate of cost is considerable and represents a great preventable burden to the health care system.
As with any scientific endeavour, a number of limitations are inherent in this work and as such certain considerations should be borne in mind when interpreting the data. Relative risk estimates used were derived from meta-analyses of observational studies. While observational studies are not the highest level of scientific evidence, meta-analysis of these studies is the best available evidence. However, these may be affected by bias such as confounding, effect modification, latency period effects, effects due to choice of reference level and exposure misclassification. Another limitation is that the relative risks used in the AAF assume that risks found in different populations are comparable and that relative risks do not vary with age. Both these assumptions may be flawed. Exposure is estimated by combining survey and per capita data. This method is used to overcome the problem of under-reporting that occurs in survey estimates. However, this method may introduce some error, such as overestimating consumption estimates in certain groups.
Healthcare costs in Ireland, as elsewhere, are escalating. We have identified alcohol as a considerable burden on hospitalisations. Much of this is preventable. The Irish population receives little protective effect from alcohol due to the detrimental Irish pattern of drinking. There must be a focus at national policy and local operational level to reduce harmful alcohol consumption in order to prevent hospitalisations and hospital costs due to alcohol.
Acknowledgements
Deirdre Goggin at the Department of Public Health, Galway; Tadhg O’Suilleabhain at the Statistics Department, AIB; Antoinette Daly and Yulia Kartalova-O’Doherty at the Health Research Board; Karen Morgan and Mark Ward at the Royal College of Surgeons in Ireland.
Correspondence: J Martin
8 Longford Terrace, Monkstown, Co Dublin
Email: [email protected]
References
1. World Health Organisation and Department of Mental Health and Substance Abuse, Noncommunicable Diseases and Mental Health Cluster. WHO global status report on alcohol 2004. 2004.
2. Ramstedt, M and Hope, A. The Irish drinking culture - drinking and drinking-related harm, a European comparison. 2003.
3. Rose G. The Strategy of Preventative Medicine.Oxford, 1992.
4. Spurling MC, Vinson DC. Alcohol-related injuries: evidence for the prevention paradox. Ann.Fam.Med. 2005;3:47-52.
5. Walter SD. The estimation and interpretation of attributable risk in health research. Biometrics 1976;32:829-49.
6. World Health Organisation and Department of Mental Health and Substance Depenence. International guide for monitoring alcohol consumption related harm. 2000.
7. Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W. Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses. Ann.Epidemiol. 2007;17:S16-S23.
8. Rehm J, Chisholm D, Room R, Lopez A. Alcohol Use. Comparative quantification of health risks. Global and regional burden of disease attribution to selected major risk factors. 2004. World Health Organisation, Geneva.
9. Morgan K, McGee H, Watson D, Perry I, Barry M, Shelley E, Harrington J, Molcho M, Layte R, Tully N, Van Lente E, Ward M, Lutomski J, Conroy R, Brugha R. SLÁN, 2007; Survey of Lifestyle, Attitudes and Nutrition in Ireland. Main Report. 2008. Department of Health and Children.
10. Mongan D, Reynolds S, Fanagan S, Long J. Health-related consequences of problem alcohol use. Overview 6. Health Research Board. 2007.
11. Cho E, Smith-Warner SA, Ritz J, van den Brandt PA, Colditz GA, Folsom AR, Freudenheim JL, Giovannucci E, Goldbohm RA, Graham S, Holmberg L, Kim DH, Malila N, Miller AB, Pietinen P, Rohan TE, Sellers TA, Speizer FE, Willett WC, Wolk A, Hunter DJ.. Alcohol intake and colorectal cancer: a pooled analysis of 8 cohort studies. Ann.Intern.Med. 2004;140:603-13.
12. Ridolfo B, Stevenson C. The quantification of drug-caused mortality and morbidity in Australia, 1998. 2001. Drug Statistics Series No. 7.
13. Martin J, Barry J, Goggin D, Morgan K, Ward M, O'Suilleabhain T. Alcohol-Attributable Mortality in Ireland. Alcohol Alcohol 2010; 45:379-386.
14. Health Atlas Ireland [videorecording]. 2010.
15. Hospital In-Patient Enquiry Scheme [videorecording]. 2010.
16. National Psychiatric In-patient Reporting System [videorecording]. 2010.
17. Xiao J, Rowe T, Somerford P, Draper G, Martin J. Impact of alcohol on the population of Western Australia. 2008. Department of Health, Western Australia.
18. Rivara FP, Garrison MM, Ebel B, McCarty CA, Christakis DA. Mortality attributable to harmful drinking in the United States, 2000. J.Stud.Alcohol 2004;65:530-536.
19. Jones L, Bellis M, Sumnall H, Tocque L. Alcohol-attributable fractions for England: Alcohol-attributable mortality and hospital admissions. 2008. Centre for Public Health, Faculty of Health and Applied Social Sciences, Liverpool, John Moores University.
20. Bedford D, O'Farrell A, Howell F. Blood alcohol levels in persons who died from accidents and suicide. Ir.Med.J. 2006;99:80-83.
21. Rehm J, Taylor B, Roerecke M, Patra J. Alcohol consumption and alcohol-attributable burden of disease in Switzerland, 2002. Int.J.Public Health 2007;52:383-92.
22. Sjogren H, Eriksson A, Brostrom G, Ahlm K. Quantification of alcohol-related mortality in Sweden. Alcohol Alcohol 2000;35:601-11.
23. Cipriani F, Balzi D, Sorso B, Buiatti E. Alcohol-related mortality in Italy. Public Health 1998;112:183-88.
24. Statistics and indicators on women and men. 2005. United Nations.
25. Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction 2003;98:1209-28
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|