|
|
|
|
|
|
|
|
P Lennon,SG Khoo,Colreavy M
|
|
|
Ir Med J. 2012 Mar;105(3):78-80
P Lennon, SG Khoo, M Colreavy
Department of Otolaryngology, Head and Neck Surgery, Mater Misericordiae University Hospital, Eccles St, Dublin 7
Abstract
We present a review of patients from Eastern Europe who have recently immigrated to Ireland with complicated otological disease. We carried out a retrospective chart review of these patients. These are a complicated cohort of 7 patients, 5 (71.4%) of whom had previous ear surgery, none had old notes and there was often a need for interpreters (3 or 42.8%) and challenging surgery. Follow up was also problematic with many of the patients. In summary this is a case series to highlight a relatively new group of patients to emphasize the need for pre-operative CT scans, facial nerve monitoring and the difficult nature of revision surgery with no old notes.
|
|
Introduction
Ireland has a long history as a country of significant emigration, but the economic boom during the 1990s brought unprecedented levels of prosperity and helped transform it into a "country of immigration." As a reflection of its relative openness to economic immigration, Ireland granted citizens of the 10 new EU member states free access to the Irish labour market immediately upon EU enlargement on May 1, 20041. The Central Statistics Office has stated that during the third quarter of 2007, an estimated 341,600 foreign nationals were residing in Ireland, with almost 60 percent of Irish work force growth from Eastern Europe2. Although undoubtedly contributing to the economic performance of the Celtic Tiger, this immigration has also led to a new interesting cohort of patients with complicated ear disease. These are recent immigrants from Eastern Europe with no details of previous surgical procedures and in general poor communication. The aim of this case series is to highlight the difficulties involved with non-English speaking patients with complicated mastoid disease and often with multiple previous surgeries. We also review the causes of failure of previous mastoid surgery and the value of pre-operative CT scans.
Methods
Our methods involved a four-year retrospective chart review, focusing on the country of origin, the anatomical reasons for failure of previous surgery, and highlighting the operative finding and difficulties of both surgery and follow-up. We examined the charts for initial presentation and past medical history, in particular previous otological surgery. Operative notes were carefully analysed to compare findings at surgery to well-established requirements for mastoid surgery failure, such as recurrent disease, incomplete exteriorization of diseased cells and poor condition of the surgical field. All patients were from Eastern European countries that have recently joined the European Union (E.U.) and those requiring minor procedures such as tympanoplasty were excluded.
Results
There were seven patients in total, four female and three male, with an age range of 29-43 years old and an average age of 34 years. Four of the patients were from Romania, and one each from Latvia, Slovakia and Poland. They presented in a variety of ways, most with chronic otorrhoea (6 patients), but also otalgia (2), poor hearing (2) and one patient with acute mastoiditis. None of the patients had old notes available, but 5 of the 7 had had previous surgery. The attic was the most common location for cholesteatoma, but disease was found in a number of anatomical areas, and in 3 patients bilaterally. Formal interpreters were required in 3 cases.
Figure 1: Bilateral disease
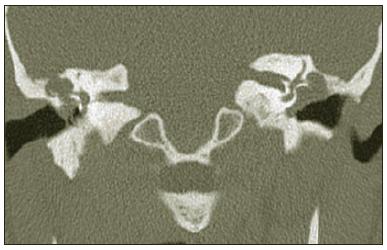
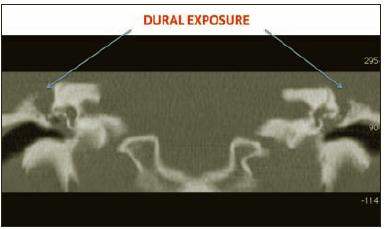
Of the 5 that had surgery in the past, 4 had previous mastoidectomies, 2 with extensive revision surgery with canal wall down mastoidectomies. Both though were found to have high facial ridges, mastoid sumps and narrow meatoplasties. At surgery six of the seven had cholesteatoma and one had tubotympanic granular disease. Significant findings included 3 with dehiscent facial nerves, 2 lateral semi-circular canal fistulaae (LSCC) and 3 patients with dural exposure. Three patients were also found to have anterior sigmoid sinuses, one in particular with no covering bone. Previous attempts at reconstruction , including a cartilage graft and a cortical strut from stapes to malleus, were also found in both patients that had had revision mastoid surgery in the past. CT scans were performed on all patients pre-operatively and examples are shown in images (Figures 1-3).
Preoperative facial nerve monitoring was used in all cases. Six of the seven had a postauricular approach, and three had a front-to-back procedure. The canal wall was taken down in five, and dural exposure was covered with Kurtz cartilage in two cases and fascia lata in one. Ossicular chain reconstruction was attempted in three patients where appropriate. Both LSCC fistulae were repaired using a fascial graft covered with Tisseel glue. Six of seven had meatoplasties. Follow-up with these patients was found to be very difficult with multiple non-attendances to outpatients and patients often missing appointments for investigations. There was often the need for interpreters, particularly in consenting pre-operatively.Post-operative audiograms revealed no 'dead ears' and no change in 5 out of 6 patients, including both patients with a LSCC fistula. One patient had a 10db hearing loss and one patient did not have a post-op audiogram due to multiple non-attendances to out-patients.
Figure 2: Close –up view
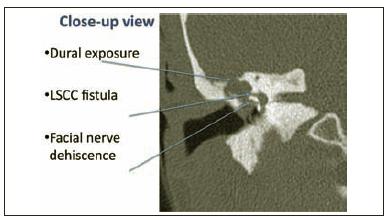
Figure 3: Extensive bilateral disease with dural exposure
Discussion
Although two of our patients presented without prior surgical intervention it was the 5 that had previous mastoid surgery who provided the greatest challenge, as revision surgery for chronic suppurative otitis media (CSOM) is more complicated and perilous than primary surgery. Gulya and Schweitzer (1992) categorized the causes of failure post-mastoidectomy as recurrent disease, incomplete exteriorization of diseased cells and the poor architecture of the surgical field. The most important factors, which promote persistent disease, are an inadequately lowered facial ridge, a stenotic meatus, bony overhangs of the cavity edges and a prominent mastoid tip3,4. In both our patients where previous canal wall procedures had been done, a high facial ridge, mastoid sump and narrow meatoplasty were found. It is usually impossible to differentiate between a true recurrence and residual disease, unless the surgeon himself has personally performed the primary operation5.
As all 5 of our patients had procedures carried out in foreign countries and no old operative notes or letters of reference were available to us this was especially difficult in our case. Incomplete mastoidectomy results in epithelium-lined peripheral cells, which later become discharging cysts and keep the cavity moist6. The areas of cells most likely to be incompletely exteriorized are the tegmental, sinodural angle, mastoid tip, facial recess and cells within the hypotympanic area7, which corresponds with our patient group. CT scans were performed on all patients prior to surgery. A number of significant anatomical abnormalities were found such as dehiscent facial nerves, dural exposure and lateral semi-circular canal fistulae. This highlights the view that CT scanning should be performed on all patients presenting with signs or symptoms of possible recurrent disease following mastoid surgery for chronic otitis media8. All patients had facial nerve monitoring during their procedure and even though there were facial nerve dehiscences, there were no post-operative palsies in the seven patients. Facial nerve stimulators have been found to be useful for predicting dehiscence in the bony facial canal during middle ear and mastoid surgery. Monitoring can help locate the facial nerve, guide the dissection and the drilling, and confirm its integrity, thereby allowing more definitive surgical treatment whilst preserving neural function9,10. Finally a significant problem in managing these patients was communication and follow-up. Histories were difficult to take and interpreters were often required, and even so there were often problems with attendance at outpatients. This is a cohort of patients comparable to chronic suppurative otitis media seen in the past in the Traveller community in Ireland and the Aboriginal community in Australia, where reports of incidence of CSOM in this group is inordinately high, running between 25 and 47%11.
In conclusion, this is a complicated cohort of patients that does however lend to opportunities to teach intricate surgery to senior trainees. We would also like to emphasize that the likely reason for failure of previous mastoid surgery include inadequate meatoplasty, high facial ridges, and failure to clear disease fully while attempting cartilage reconstruction. We would also like to stress the importance of pre-operative CT scanning, facial nerve monitoring and highlight the challenges of communication and follow-up in a non-English speaking cohort of patients with chronic suppurative otitis media.
Correspondence: P Lennon
15 The Orchards, Courtbrack Avenue, Limerick
Email: [email protected]
References
1. Ruhs M. Ireland: A Crash Course in Immigration. http://www.migrationinformation.org/Profiles. Accessed 10/01/2010 2
2. Central Statistics Office, Ireland. http://www.cso.ie/. Accessed 10/01/2010.
3. Gulya AJ. Revision mastoid surgery. Operative techniques in Otolaryngology-Head and Neck Surgery. 1992;3:39-4 2.
4. Goldenberg RA. Sink-trap effect as a cause of failure in mastoidectomy. Laryngoscope. Oct 1988;98:1143-11 44.
5. Glasscock ME, 3rd. Surgical management of the previously operated chronic ear. In: Tos M, ed. Cholesteatoma a nd Mastoid Surgery: Amsterdam/Berkeley/Milano; 1989:1027-1032.
6. Pillsbury HC, 3rd, Carrasco VN. Revision mastoidectomy. Arch Otolaryngol Head Neck Surg. Sep 1990;116:1019 -1022.
7. Nadol JB, Jr. Causes of failure of mastoidectomy for chronic otitis media. Laryngoscope. Apr 1985;95:410-4 13.
8. Campbell JP, Pillsbury HC, 3rd. The use of computerized tomographic imaging in revision mastoid surgery for c hronic otitis media. Am J Otol. Nov 1990;11:387-394.
9. Silverstein H, Smouha E, Jones R. Routine identification of the facial nerve using electrical stimulation dur ing otological and neurotological surgery. Laryngoscope. Jul 1988;98:726-730.
10. Noss RS, Lalwani AK, Yingling CD. Facial nerve monitoring in middle ear and mastoid surgery. Laryngoscope. M ay 2001;111:831-836.
11. Jeffries-Stokes C, Lehmann D, Johnston J, et al. Aboriginal perspective on middle ear disease in the arid zo ne of Western Australia. J Paediatr Child Health. May-Jun 2004;40:258-264.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|