|
|
|
|
|
|
|
|
IM Collins,L Fay,MJ Kennedy
|
|
|
|
Ir Med J. 2011 Jan;104(1):6-9.
|
|
IM Collins, L Fay, MJ Kennedy
Department of Medical Oncology, St James’s Hospital, Dublin 8
Abstract
The potential effect on fertility for patients undergoing cancer treatments is an important issue. The aim of this study was to assess awareness of fertility preservation strategies among cancer specialists involved in the management of young women with malignancy. A 10 question survey was sent to 94 cancer specialists in Ireland, comprising 28 medical oncologists, 32 haematologists and 34 breast surgeons, assessing awareness of; guidelines, facilities in Ireland, and potential barriers to referral. Fifty of 94 responded (53% response rate). Awareness of current success rates associated with assisted reproductive therapy was poor. Ten respondents (20%) indentified the estimated time delay to the delivery of chemotherapy due to fertility preservation. Three important potential barriers to referral were identified; time delays, poor prognosis disease and clinical features of the cancer. Awareness of the impact of reduced fertility is important in these patients but early consideration is vital.
Introduction
As treatments for cancers improve, physicians treating patients with cancer are becoming increasingly aware of the long-term effects of their treatments. This is a widespread issue with 22% of patients with breast cancer under 50 years of age at diagnosis1. Chemotherapy treatment carries a significant risk of ovarian failure as well as premature menopause in women of childbearing years. The most important factor in this risk is the age of the patient at the time of treatment, but the type of chemotherapy agents used also has an effect. Prevention of loss of reproductive function is difficult with no good evidence for effective preventative measures. The preservation of fertility for younger patients is an important aspect of cancer survivorship. This can be achieved with relative ease in male patients through semen cryopreservation and, although more complex the cryopreservation of embryos, oocytes, or ovarian tissue in females. The largest group of these patients are those with breast cancer, but those with haematological cancers are also included in this study. The aim was to assess levels of awareness of fertility preservation among specialists involved in the diagnosis and care of patients with cancer in Ireland who are of childbearing potential.
Methods
A questionnaire was sent to 94 cancer specialists comprising 28 medical oncologists, 32 haematologists and 34 breast surgeons. All were involved in the diagnosis or treatment of cancer in pre-menopausal women potentially for treatment with chemotherapy. A list of all those actively treating these patients was available through national speciality groups. The questionnaire evaluated the respondent’s awareness of guidelines and current practice in fertility preservation, awareness of available facilities and estimated outcomes for assisted fertility for women. It examined the level of importance attached to various reported barriers to offering fertility preservation. The questionnaire comprised 10 questions in a single page format designed to minimise the time to complete the survey and thus maximise response rates, and thus confidence in the study findings. The authors developed this survey based on a review of the literature and previous qualitative interviews2-4 and this was piloted among a small number of physicians, some of who later participated in the survey. A combination of multiple-choice questions and ranking questions were used to give a forced choice, avoiding ambiguous answers.
A commercial, online survey tool (www.surveymonkey.com) was used for hosting the web-based survey and for data entry, collation and basic statistical analysis. SPSS statistical package, version 18 was used for further statistical analysis. An initial email was sent explaining the purpose of the study and a copy of the questionnaire as well as a link to a web-based version was included. This was followed up with a paper version 1 week later. A pre-addressed envelope was included in the correspondence. Non-responders received a further request for participation and a paper version 4 weeks later. Just 6 responders completed the online version, the remaining 44 replied by post. As the questionnaire was anonymous, no subset analysis could be preformed on responders within the different specialties.
Results
Of 94 questionnaires sent, 50 responses were received (a 53% response rate). Of these 31 (62%) were aware of some of the available international guidelines on the preservation of fertility in young patients undergoing chemotherapy. This included 28 aware of ASCO guidelines6, 10 of ESMO guidelines7 and 7 aware of the Royal College of Physicians and Gynaecologists guidelines8. Many were aware of more than one set of recommendations. Among those replying, 41(82%) routinely referred men for sperm banking, reflecting the relative ease of preservation of male fertility. As sperm banking is available with little delay, and good subsequent success rates where sperm is used, it can often be seen as a standard element before therapy. All those who responded treat women of childbearing potential but only 42 (84% responders) would routinely discuss fertility with these women. International guidelines would suggest that all patients should have fertility discussed before treatment. Twenty one (46%) reported using GnRH agonists as a measure to protect ovarian function. These agents have been widely used in an attempt to suppress ovarian function and to prevent damage to the follicles at a sensitive stage in their maturation, despite a lack of evidence for their use.5
Awareness of current outcomes for assisted fertility was poor, with just 42% (18) aware of conventional IVF success rates, 21% (9) for frozen embryo and 26% (11) for frozen oocyte success rates (Table 1). While 85% (41) correctly estimated costs involved (currently approximately €5000 in Ireland), just 2% were aware of the seven sites offering treatment in Ireland. While there is only one centre in receipt of state funding, six privately funded centres have indicated a willingness to treat cancer patients.
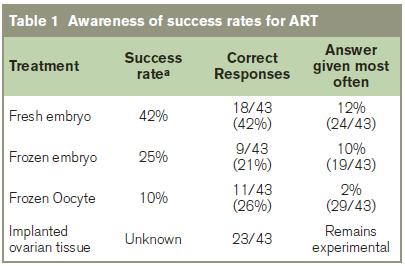
a. Average pregnancy rates in a woman less than 38 years5.
Only 20%(10) indentified the estimated time delay involved, 4-6 weeks using accelerated ovarian stimulation following interruption of a cycle. The remainder over-estimated the delay involved. This is of great clinical importance when we look at the barriers to referral for consideration of ART.
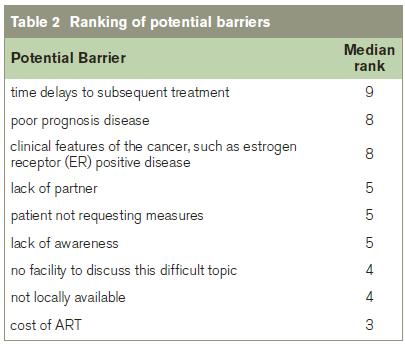
We asked responders to rank nine barriers to referral for fertility preservation in order of importance with 1 as very important and 9 as unimportant. These barriers were taken from international assessments of physicians reported barriers to referral4 (Table 2). There was a large degree of agreement on the barriers to referral, with the majority of responders identifying the same three most important factors, “time delays to subsequent treatment”, “poor prognosis disease” and “clinical features of the cancer, such as estrogen receptor (ER) positive disease”. These factors had a median score of 1, 2 and 2 respectively. Potential barriers of “lack of partner”, “patient not requesting measures” and “lack of awareness”, all had a median score of 5, while further potential barriers “no facility to discuss this difficult topic”, “not locally available” and “cost of ART” had median scores of 4, 4 and 3 suggesting they are less important. Thus, patient dependant factors would appear to be more important than psychosocial factors.
Discussion
Consensus guidelines increasingly recommend adjuvant chemotherapy for younger women with breast cancer, with women under 50 years deriving the greatest benefit from chemotherapy and 22% of patients are under 50 at diagnosis9. However 30-50% of women who receive chemotherapy for breast cancer in their 30’s and 50-100% of those treated in their 40’s will experience a premature menopause or ovarian failure and be rendered infertile8. The risk of diminished ovarian reserve increases with age, particularly over 38 years but also with the use of certain chemotherapeutic drugs, in particular alkylating agents. Other reported factors include; the dose of drugs, radiotherapy (risk is associated with dose and area treated) and combined chemoradiation10. In some instances, this may be a temporary phenomenon with menstruation recovering months to years later; however even if menses should return after treatment, menopause may occur 5-10 years earlier than expected. While the endocrine effects on early menopause can be treated, the reproductive effects are not amenable to manipulation. Premature menopause is an important survivorship issue particularly in those women who hope to preserve fertility following treatment. While women are offered the best available therapy to treat their cancer, it is also important that other aspects of their care, such as fertility preservation, be considered.
In our study, awareness is highlighted as being an issue, particularly in surgeons who need to discuss fertility at the time of diagnosis. Only 84% in our study reported discussing fertility with their patients. This mirrors an earlier study on awareness of male fertility services in oncology patients in 200311, and suggests that the improvements seen in male fertility preservation are now needed in females. The response rate of 53% is not unexpected though it may be a potential source of bias as those more aware of fertility issues are more likely to respond, however, the results and response rate are similar to a recent international study in this area3. One of the difficulties with the discussion of the risk of infertility is the lack of good quantitative data on the risks associated with specific regimens. Chemotherapy induced amenorrhea (CIA) has been used as a surrogate marker for loss of fertility, but does not accurately reflect ovarian reserve. Newer markers of ovarian function such as AMH (anti-müllerian hormone) may be able to provide better data on the true effects on ovarian function12.
Pregnancy rates, with assisted reproduction technology (ART) have improved greatly over recent years. These improvements may be the reason for the underestimation of our cohort of reported outcomes with ART. Published data5 would suggest rates of 25% for frozen embryo transfer and 5-15% for frozen oocytes, the methods used most commonly in patients due to undergo chemotherapy. The most important factor is age of the patient, with highest success rates in those under 38 years. While success rates may vary in different centres, results are consistently higher than predicted by respondents.
Current options for fertility preservation include embryo, oocyte and ovarian tissue cryopreservation with later re-implantation. All have both advantages and difficulties. Embryo preservation is the most successful but requires a donor for fertilization. Approximately 70% of frozen embryos survive freezing and thawing again. Oocyte preservation has a lower success rate due to cryobiology but advances in this area, such as the first reported pregnancy following in-vitro maturation of cryopreserved oocytes in 200913 are promising. Cryopreserved oocytes undergo in-vitro maturation at a later stage with re-implantation14, this does not require FSH stimulation there-by avoiding high estradiol levels15. The use of ovarian tissue is reporting individual case successes and will be of greater importance in the future. Seven live births have been reported to date, with the first in 200416. Both techniques may be available in the future to all females affected with cancer
Ovarian stimulation is associated with marked increase in estradiol levels sometimes up to 20 times of the levels seen in natural cycles17. Because of the large body of data implicating oestrogen and oestrogen metabolites in breast cancer there is a reluctance to treat patients with ER positive tumours with hyperstimualtion. However, these levels are short lived and there has been no proven association between ART and worse prognosis. Again this area was highlighted by our responders as an area of concern, but it remains under-evaluated and further research is needed to clarify true risks involved.
The time involved in ovarian stimulation and oocyte retrieval has improved and stimulation can take between 14 days and 6 weeks with current strategies. This was greatly overestimated in our study with only 20% of specialists aware of the time involved. This is of great importance when we consider that many see time delay to subsequent treatment a major barrier to ART. Our study clearly suggests that patient related factors are far greater barriers to ART referral than psychosocial barriers such as cost and availability, in our country at least. These need to be examined more closely in the light of available evidence. Our study would suggest that reported barriers can be overcome, and as this is of such importance to our patients, awareness of the issues and continuing education regarding options, to physicians and patients, is vital. This is certainly an area of growing importance and further research is needed.
Correspondence: IM Collins
Department of Medical Oncology, St James’s Hospital, Dublin 8
Email: [email protected]
References
1. Walshe JM, Denduluri N, Swain SM. Amenorrhea in Premenopausal Women After Adjuvant Chemotherapy for Breast Cancer. J Clin Oncol. 2006 December 20, 2006;24:5769-79.
2. Patel A, Sreedevi M, Malapati R, Sutaria R, Schoenhage MB, Patel AR, Radeke EK, Zaren HA. Reproductive health assessment for women with cancer: a pilot study. Am J Obstet Gynecol. 2009 Aug;201:191 e1-4.
3. Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Bepler G, Lancaster J, Keefe DL, Albrecht TL. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009 Dec 10;27:5952-7.
4. Quinn G, Vadaparampil S, Gwede C, Miree C, King L, Clayton H, Wilson C, Munster P. Discussion of fertility preservation with newly diagnosed patients: oncologists’ views. Journal of Cancer Survivorship. 2007;1:146-55.
5. ESHRA Assisted reproductive technology and intrauterine inseminations in Europe, 2006. 2010 [June 2010]; Available from: http://www.eshre.eu/ESHRE/English/Guidelines-Legal/ART-fact-sheet/page.aspx/1061.
6. Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, Beck LN, Brennan LV, Oktay K. American Society of Clinical Oncology Recommendations on Fertility Preservation in Cancer Patients. J Clin Oncol. 2006 June 20, 2006;24:2917-31.
7. Pentheroudakis G, Pavlidis N, Castiglione M, On behalf of the ESMO Guidelines Working Group. Cancer, fertility and pregnancy: ESMO Clinical Recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2009 May 1, 2009;20:iv178-81.
8. Royal College of Physicians TRCoR, Royal, Gynaecologists CoOa. The effects of cancer treatment on reproductive functions: Guidance on management. 2007.
9. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687-717.
10. Wallace W, Anderson R, Irvine D. Fertility preservation for young patients with cancer: who is at risk and what can be offered? Lancet Oncol. 2005 Apr;6:209-18.
11. Allen C, Keane D, Harrison RF. A survey of Irish consultants regarding awareness of sperm freezing and assisted reproduction. Ir Med J. 2003 Jan;96:23-5.
12. Jeruss JS, Woodruff TK. Preservation of Fertility in Patients with Cancer. N Engl J Med. 2009 February 26, 2009;360:902-11.
13. Chian RC, Gilbert L, Huang JY, Demirtas E, Holzer H, Benjamin A, Buckett WM, Tulandi T, Tan SL. Live birth after vitrification of in vitro matured human oocytes. Fertil Steril. 2009 Feb;91:372-6.
14. Donnez J. Advances in fertility preservation for children and adolescents with cancer. European Journal of Cancer. 2009;45:418-.
15. Dowling-Lacey D, Jones E, Bocca S, Stadtmauer L, Gibbons W, Oehninger S. Two singleton live births after the transfer of cryopreserved-thawed day-3 embryos following an unstimulated in-vitro oocyte maturation cycle. Reprod Biomed Online. 2009 Dec 11.
16. Donnez J, Dolmans MM, Demylle D, Jadoul P, Pirard C, Squifflet J, Martinez-Madrid B, Van Langendonckt A. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004;364:1405-10.
17. Azim AA, Costantini-Ferrando M, Oktay K. Safety of Fertility Preservation by Ovarian Stimulation With Letrozole and Gonadotropins in Patients With Breast Cancer: A Prospective Controlled Study. J Clin Oncol. 2008 June 1, 2008;26:2630-5.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|