|
|
|
|
|
|
|
|
O O'Toole,Ciara Mahon,Karen Lynch,FM Brett
|
|
|
|
Ir Med J. 2009 Jul-Aug;102(7):207-9.
|
O O'Toole, C Mahon, K Lynch, FM Brett
Department of Neuropathology, Beaumont Hospital, Beaumont, Dublin 9
Abstract
Alcohol consumption in Ireland has nearly doubled during the period 1989-2001. To evaluate the relationship of alcohol to fatal head injuries in the acute hospital setting we created a data base of all fatal traumatic brain injuries in the Department of Neuropathology at Beaumont Hospital over a ten year period (1997-2006 inclusive). 498 cases were identified (351 males: 147 females). Fatalities were highest in males aged 19-25 years (N=101) and 51-70 years (N=109). Falls (N=210) and road traffic accidents (N=183) were the commonest modes of presentation. 36/210(17%) falls had positive blood alcohol testing, 9/210(4.3%) had documentation of alcohol in notes but no testing, 35/210 (16.7%) tested negative for alcohol and 130/210(61.9%) were not tested. The RTA group (N=183) comprised drivers (n=79), passengers (n=47) and pedestrians (n=57). 65/79 (82.2%) of drivers were males aged 19-25 years. Blood alcohol was only available in 27/79 (34.1%) drivers and was positive in 13/27(48.1%). 14/75 (18.7%) pedestrians were tested for alcohol, 4/14(28.6%) were positive. Overall 142/183 (77.6%) of the RTA group were not tested. The contribution of alcohol to fatal traumatic brain injuries is probably being underestimated due to omission of blood alcohol concentration testing on admission to hospital. Absence of national guidelines on blood alcohol testing in the emergency department compounds the problem.
Introduction
Alcohol consumption is a major contributory factor in the attendances of many patients at hospital Emergency Departments in the Dublin area1. However, if a driver is injured in a road traffic accident (RTA) and taken to the Emergency Department (ED), medical treatment takes precedence over blood alcohol testing (BAC). This situation is not unique to Ireland2,3. If BAC is not recorded at the time of admission it is unlikely that it will be measured or recorded at any other stage4. This has important legal implications, whether the patient survives or dies5-7. There is little information available in Ireland about BAC in those who sustain fatal traumatic brain injuries in the acute hospital setting. This study was undertaken to ascertain the role of alcohol in fatal traumatic brain injuries by reviewing autopsy and toxicology records and interviewing consultants in emergency medicine.
Methods
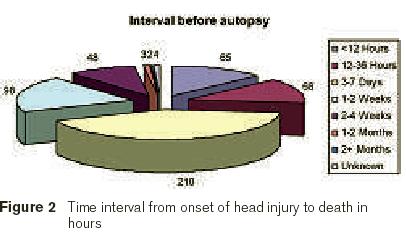
Autopsy records from 1997 up to, and including, 2006 (N = 498) in the Department of Clinical Neurological Sciences at Beaumont Hospital, a large acute teaching hospital in Dublin, were reviewed for cases coded as “traumatic brain injury”. The cases selected were those where the hospital coding included the terms “headache, fall, assault, road traffic accident, suicide, or unknown”. A data base was then created using Microsoft Access. The gender, age, interval from presentation to death, mechanism of injury, cause of death and BAC were all recorded. The interval from presentation to death was looked at specifically to ascertain any delay between the incident and subsequent death. If there was a delay the BAC at autopsy would be irrelevant, whereas the BAC at presentation would be important.
Particular attention was paid to falls and road traffic accidents as these were the commonest cause of (Fatal Traumatic Brain Injuries) FTBI. If the patient was dead on arrival in the Emergency Department the BAC was obtained from the autopsy reports. Where there was a delay from admission to death the admission BAC was sought by checking the “live and deceased” databases in the Toxicology Department of Beaumont Hospital. Blood alcohol concentration (BAC) in Ireland is measured in milligrammes of alcohol per mililitre of blood. A concentration of 1 gramme alcohol per 1 millilitre of blood yields a BAC of 100%. Because alcohol is known to impair judgment at levels lower than the legal limit the presence of any alcohol in the blood samples was considered a “positive” case8,9. Additionally consultants in emergency medicine from major trauma centres in Dublin (i.e. Beaumont, St Vincent’s, Mater Hospitals and Drogheda were interviewed to ascertain policies on BAC testing).
Results
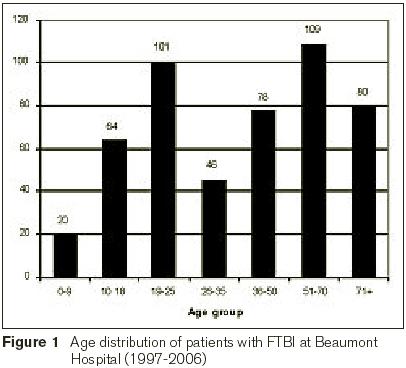
498 cases (351 M :147 F) fulfilled the criteria for inclusion in the FTBI data base. The highest number of fatalities were in males in the age groups 51 -70 years (N =109) and 19-25 (N =101) (Figure 1). The majority of cases died in hospital 3-7 days after admission (Figure 2). The positive BAC samples ranged from <100 to > 500 mg%.
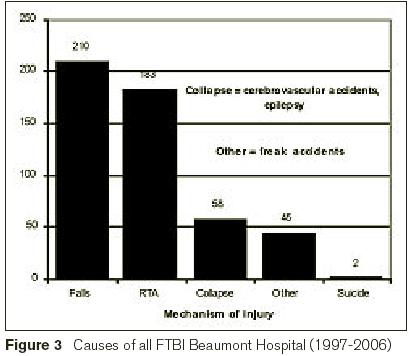
Falls (210) (M =155; F=55) were the commonest mechanism of fatal injury, followed by road traffic accidents (RTAs) (183) (Figure 3). The majority of falls occurred in males in the age group 51-70 years. A documented association with alcohol consumption was found in 45/210(21.4%) cases (M 31; F14), 36/210(17%) had a positive BAC and in 9/210(4.3%) cases alcohol was deemed to be a contributing factor in the medical notes although BAC was not measured. Three patients who tested positive were in the age range 10-18 years. Of the remaining 165 cases 35(16.7%) were scrutinised and were found to be negative. In 139/210(66.2%) cases no record was found in the database base in the Toxicology Department.
RTA’s accounted for 183 cases – drivers (n=79), passengers (n=47), pedestrians (n=57).65/79(82.22%) drivers were males in the age group 19-25 years. Documented BAC was available in only 27/79(34.1%) drivers (one aged 10-18 years) and was positive in 13/27(48.1%) cases (all males). In a further 2 cases BAC was not recorded but the medical notes mention alcohol as a “contributing factor”. 14/57(24.6%) Of pedestrians had BAC testing, 4/14(28.6%) were positive and a further 2 cases had documentation of recent alcohol use in the notes but no BAC was checked. Two pedestrians with a positive BAC were in the age group 10-18 years. 142/183(77.6%) RTA cases had no record of BAC. From the survey of consultants in emergency medicine in the major trauma hospitals in Dublin and Drogheda we found that BAC levels were not routinely taken even in cases where patients were admitted with suspected alcohol-related head injuries.
Discussion
One in four (25%) patients attending hospital emergency departments in the Dublin area have alcohol-related diagnoses and one in eight patients (13%) are clinically intoxicated at the time of attendance1. BAC was positive in 13% of our RTA and falls fatalities though only 28% of this population were actually tested, suggesting that the true contribution of alcohol may be higher. Most of our cases came to autopsy 3-7 days after admission at which stage testing for BAC is futile. Only the “admission” BAC would have been of value in these cases but it was not estimated in 72% (of cases). The peak incidence of falls was in males in the age group 51-70 years (Figure 3). The association between older males, alcohol consumption and fatal falls is well documented in the literature10. At the same peak BAC the postural balance in older people is more impaired than in their younger counterparts11. Physiological factors, co-existent disease and medication make older adults more vulnerable to the effects of alcohol with consequent falls and other mechanisms of injury10,11. Alcohol-related falls, in general, are associated with a greater incidence of head injuries and a greater severity of the resulting injury12. RTA’s (N=183) were the second commonest cause of FTBI’s in our study (Figure 3). The peak age distribution of drivers was in males in the age group 19-25. Compared with drivers aged over 30, teenage male drivers have five times the risk and drivers in their twenties three times the risk of injury at all BAC levels13. Thirteen drivers and 4 pedestrians had positive BAC. Medical notes suggested alcohol as a contributing factor in a further 2 drivers and 2 pedestrians although BAC was not measured. No BAC data were available on passengers.
There are no national BAC testing guidelines for emergency physicians in Ireland. Confidentiality and ethical issues arise with respect to BAC testing, a situation that is not unique to Ireland2,3. If BAC is measured or estimated on admission and is elevated, this figure has medical and legal implications. However, if a BAC is not checked at the time of admission, it is unlikely to be tested at all4 and thus the contribution of ‘alleged’ alcohol consumption to the resulting injury remains unknown. This raises a number of interesting ethical questions: Is there a moral obligation to document BAC in the emergency department?; If so, which patients should be tested? Can a conscious but inebriated patient with a head injury give informed consent for BAC testing? Should physicians have the right to test BAC in an unconscious patient without their consent? In the UK, BAC can only be measured in an unconscious patient if the attending physician immediately in charge of the case does not object14. In the USA, forensic blood samples may be taken from an unconscious patient. It could be argued that BAC testing in a comatose head injury patient is entirely reasonable and indeed “standard practice”.
Both the American College of Emergency Physicians and the American College of Surgeons recommend the routine toxicological screening of all trauma victims admitted to trauma centres15. The Royal College of Surgeons in Ireland recommends ‘sometimes’ sending toxicology as an adjunct to the primary survey in a severely injured patient16. Screening injured patients for alcohol problems and providing intervention has been shown to be beneficial in reducing alcohol use and alcohol re-admissions in the USA17. In theory, this sounds like a good idea but the majority of trauma centres in the USA do not screen injured patients18. One potential barrier in the US is that performing a BAC or urine toxicology screen on an injured patient may result in the insurance company denying payment if the test is positive.
The consultants in emergency medicine who were interviewed for this study highlighted a number of practical barriers to routine BAC testing. (1) BAC testing not considered of benefit to the immediate management of patients with head injury. (2) Concern that undue attention to or over-interpretation of a high alcohol level might lead to other causes of altered mental status or acute neurological deterioration being overlooked. (3) Apprehension with regards to the legal issues of consent in obtaining a sample. (4) Blood contamination by use of ethanol containing swabs during withdrawal. The current infrequency of blood alcohol testing in accident and emergency departments makes it impossible to precisely estimate the contribution of alcohol to FTBI’s. BAC testing is a controversial topic amongst consultants in emergency medicine for valid reasons. There is a need for debate with regards to clear national guidelines on BAC testing in the emergency department setting.
Acknowledgements
Thanks to the departments of Neuropathology, Emergency Medicine and Toxicology, Beaumont Hospital, Dublin 9 and the participating Emergency departments of St Vincents Hospital, Dublin 4, the Mater Misericordiae Hospital, Dublin 7 and Our Ladys' Hospital, Drogheda, Co Louth.
Correspondence: FM Brett
Department of Neuropathology, Beaumont Hospital, Beaumont, Dublin 9
Email: [email protected]
References
1. Hope, A., et al., Alcohol and injuries in the accident and emergency department – a national perspective Dublin. Department of Health and Children 2005.
2. Higuchi, A., et al., Problems in blood alcohol testing of severely injured drivers brought to emergency departments in Japan. Leg Med (Tokyo), 2005. 7: 299-305.
3. Schermer, C.R., et al., Intoxicated motor vehicle passengers warrant screening and treatment similar to intoxicated drivers. J Trauma, 2001. 51: 1083-6.
4. Biffl, W.L., et al., Legal prosecution of alcohol-impaired drivers admitted to a level I trauma center in Rhode Island. J Trauma, 2004. 56: 24-9.
5. Bell, G. and A. Cremona, Alcohol and death certification: influencing current practice and attitudes. Br J Addict, 1989. 84: 1523-5.
6. IAEM, Submission to the road safety authority for consideration in respect of road safety strategy 2001-2011. Royal College of Surgeons in Ireland, 2006.
7. National association of insurance commissioners: Model regulation service. Kansa City, M., NAIC model laws regulations and guidelines. Uniform individual accident and sickness policy provisions law, 2004. 11: 180-181.
8. Bellis, M., M. Bolster, A., and C.T. Doyle, The role of alcohol in deaths presenting to the coroner's service in Cork City and County. Irish Medical Journal, 2009. 102: 13-15.
9. Compton RP, B.R., Moscowitz H et al, n: Mahew DR, Dussault C, eds. Proceedings of the 16th International Conference on Alcohol, Drugs and Traffic Safety, Montreal 4-9 August. Montral, Societe de l’assurance automobile du Quebec 2002:39-44.
10. Sorock, G.S., et al., Alcohol-drinking history and fatal injury in older adults. Alcohol, 2006. 40: 193-9.
11. Vogel-Sprott, M. and P. Barrett, Age, drinking habits and the effects of alcohol. J Stud Alcohol, 1984. 45: 517-21.
12. Johnston, J.J. and S.J. McGovern, Alcohol related falls: an interesting pattern of injuries. Emerg Med J, 2004. 21: 185-8.
13. Keall, M.D., W.J. Frith, and T.L. Patterson, The influence of alcohol, age and number of passengers on the night-time risk of driver fatal injury in New Zealand. Accid Anal Prev, 2004. 36: 49-61.
14. Stark and M.M., Clinical Forensic Medice. A Physician’s guide. Humana Press, Totowa, New Jersey, USA, 2005.
15. Soderstrom, C.A., J.T. Dailey, and T.J. Kerns, Alcohol and other drugs: an assessment of testing and clinical practices in U.S. trauma centers. J Trauma, 1994. 36: 68-73.
16. O' Higgins, N., et al., RCSI guidelines: initial management of the severely injured patient. Royal College of Surgeons in Ireland, 2003: 16.
17. Gentilello, L.M., et al., Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg, 1999. 230: 473-80; discussion 480-3.
18. Gentilello, L.M., et al., Effect of the Uniform Accident and Sickness Policy Provision Law on alcohol screening and intervention in trauma centers. J Trauma, 2005. 59: 624-31.
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|