Abstract
This study describes the demographics and treatment status of HIV-infected adults accessing ambulatory care in the Republic of Ireland and estimates diagnosed HIV prevalence rates. 3254 HIV-infected adults attended 1 of the 6 specialist HIV centres in the 12-month period 1st July 2009 to 30th June 2010. 2023/3254 (62%) were male, 1761/3133 (56%) Irish and 1048/3133 (34%) African. 1924/3098 (62%) resided in the Dublin area. The mean age was 39.8 years (SD 9.3); probable route of acquisition was available for 2898/3254 (89%); heterosexual acquisition accounted for 1442 (50%), MSM 777 (27%) and IDU 598 (21%). 2574/3202 (80%) were on highly active antiretroviral therapy (HAART).Of these 87% had HIV-RNA levels < 50cpm and 94% < 500cpm. The HIV diagnosed prevalence rate is estimated at 1.09/1000 nationally and at 2.25/1000 in the Dublin area for 15-59 year olds
Introduction
Highly active antiretroviral treatment (HAART) has reduced the morbidity and mortality associated with Human Immunodeficiency Virus (HIV) infection; it can also prevent onward transmission when HIV RNA level is suppressed.1,2 At an individual level disease management aims to diagnose infection at an early stage and engage patients in specialist care. At a societal level the focus is to provide timely disease surveillance and prevent onward transmission by an expanded HIV test and treat approach.3 In Ireland, the Health Protection Surveillance Centre (HPSC) collates demographic data on newly diagnosed HIV infections and reported 344 new diagnoses during 2013 bringing the cumulative number reported as newly diagnosed to 6979 since the early 1980s.4 This information is valuable, however the demographics and clinical status of patients living with HIV infection in Ireland have not been previously described. This contrasts with the United Kingdom (UK), where Public Health England carries out an annual Survey of the Prevalence of HIV-Infections Diagnosed (SOPHID).5 SOPHID, soon to be replaced by the HIV and AIDS reporting system (HARS), informs each primary care trust of their diagnosed HIV prevalence rates and reports regular demographic data. Such data and prevalence rates in Ireland were previously unknown. In 2008, in an effort to reduce the number of late presentations the UK HIV testing guidelines were published; HIV diagnosed prevalence rates informed the cut-off at which routine testing for HIV in healthcare settings was recommended.6 In areas of high diagnosed HIV prevalence (> than 2/1000 of population aged 15-59) it is assumed that there is a corresponding high undiagnosed prevalence rate; audit data from the United Kingdom have reported it as high as 28%.7 In these circumstances US data has shown the introduction of opt out screening in healthcare settings is cost effective.8 This study was undertaken to describe the demographics and treatment status of HIV infected adults accessing ambulatory care in the Republic of Ireland and to estimate the diagnosed prevalence of HIV.
Methods
There are six sites for specialist adult (17 or over) HIV care in Ireland, three in Dublin: St James's Hospital, Mater Misericordiae University Hospital and Beaumont Hospital and three outside: Cork University Hospital, Galway University Hospital and Limerick Regional Hospital. All newly diagnosed patients are referred to one of these centres for care. The primary objective was to retrospectively identify the number of patients accessing specialist ambulatory care for HIV-infection in Ireland (PACHI) over a 12-month period from July 2009 to June 2010. Secondary objectives included: to record demographics; to record the attendances of each patient over the 12-month period; to collect antiretroviral treatment (ART) data; to evaluate virological suppression in those on ART and using Irish 2011 population census data estimate diagnosed prevalence rates for people living with HIV in Ireland as a whole and by region. Ethical approval was sought at each individual centre. Data were pseudonymised and collated on an encrypted laptop provided by the HPSC. Pseudonymisation created a unique code for each individual using initials and date of birth to allow comparison across sites and prevent potential duplication. Consent was not obtained from individual patients as all information gathered was from existing data sources and no individual patient identifiers were retained. Cases were retrospectively identified using existing primary clinic datasets. Patients who attended at least one HIV specialist outpatient appointment (physician-led) at one of the 6 centres from 1st July 2009 to 30th June 2010 met the inclusion criteria. One investigator carried out all the data collection to maintain the reliability of the process. Demographics (gender, age, county of residence, country of birth, probable route of acquisition) and the number of outpatient attendances in the 12-month period were retrospectively manually extracted from primary clinic datasets, the hospital administration systems or electronic patient records wherever the data was available. Most recent CD4 count and HIV RNA level were extracted from primary datasets or computerized laboratory systems depending on the centre. Pharmacy data were extracted from either paper records or pharmacy datasets depending on the site. An encrypted database was created for each site; the data collection process had to be customised at each site due to the differing Information Technology systems in existence across the 6 different hospital sites. A data dictionary was used from the initiation of the study.
On completion of the study the 6 databases were merged into SPSS for analysis. HIV diagnosed prevalence rates for Ireland and each county were estimated using 2011 population census data9 as a denominator. Data were primarily descriptive. Independent samples T test was used to compare mean ages of males and females. Further analysis was performed looking at numbers on antiretroviral treatment and viral suppression rates defined as HIV RNA level < 50 cpm. For categorical variables: gender, country of origin and probable route of acquisition chi square analysis was performed and for parametric variables: mean age and mean recent CD4 cell count analysis was performed using independent samples t test. The number of outpatient visits were analysed using the Mann Whitney U test.
Results
Demographics
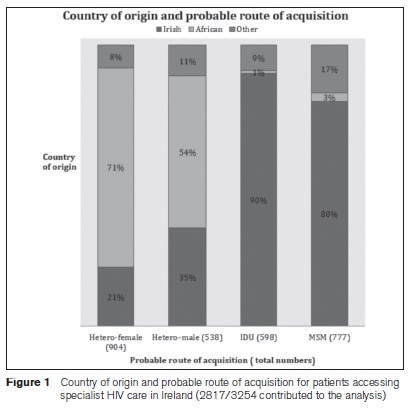
Over the 12-month period 3254 patients were identified as accessing specialist ambulatory care for HIV infection in Ireland. 2642 (81.1%) accessed care in Dublin: St James’s Hospital 1745 (53.6%), Mater Misericordiae University Hospital 538 (16.5%), Beaumont Hospital 359 (11.0%), whilst 612 (18.8%) accessed care outside: Cork University Hospital 365 (11.2%), University College Hospital Galway 170 (5.2%) and Limerick Regional Hospital 77 (2.4%). 2023 (62.2%) were male. Country of origin was available for 3133 (96.3%): 1761 (56.2%) were Irish; 1048 (33.5%) African; 133 (4.3%) from Eastern Europe; 107 (3.4%) from Western Europe; 36 (1.2%) from Asia and 48 (1.5%) from another region. Probable route of acquisition was available for 2898 (89.1%):heterosexual acquisition accounted for 1442 cases (49.8%); men having sex with men (MSM) 777 cases (26.8%) and injecting drug users (IDU) 598 cases (20.6%).(Figure 1).
Age
Overall the mean age was 39.8 (standard deviation, SD 9.3): the mean age for males was 41.5 (SD 9.7), which was significantly older than the mean age for females of 37 (SD 8.1). (P value < 0.001, 95% confidence interval (CI) 3.8-5.1.)
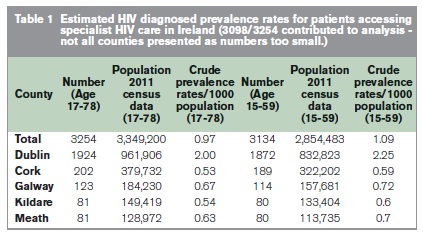
Prevalence
Using 2011 population census data for ages 17-78 (age range of this cohort) and ages15-59 (age range reported internationally) as denominators, HIV diagnosed prevalence rates are estimated by county. In the Republic of Ireland the overall HIV diagnosed prevalence rate is estimated at 0.97/1000 and 1.09/1000 for ages 17-78 and 15-59 respectively. County of residence data were collected on 3098 cases and in the Dublin area the HIV diagnosed prevalence rate is estimated at 2.0/1000 and 2.25/1000 for ages 17-78 and 15-59 respectively (Table 1).
Outpatient Department (OPD) Attendances
The median number of OPD attendances per patient in the twelve-month study period was 4 (Interquartile range IQR 2). 569/3251 patients (17.5%) attended OPD 6 or more times in the twelve-month period. 94/777 (12.1%) of MSMs, 81/538(15.1%) of male heterosexuals, 147/598 (24.6%) of IDUs and 187/904 (20.7%) female heterosexuals attended 6 or more times.
Antiretroviral Treatment (ART)
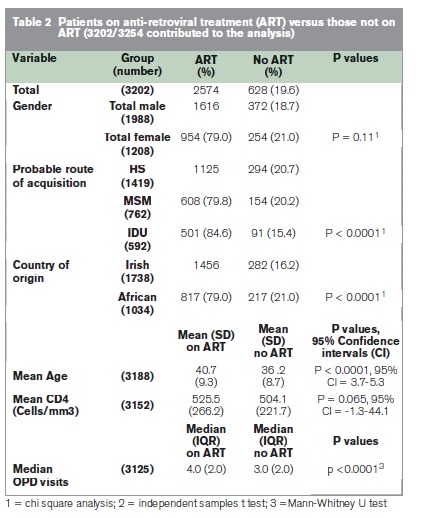
Accurate ART data was available on 3202 (98.4%) patients. 2574/3202 (80.4%) were on ART. Those on ART were older; 40.7 v 36.2 years p < 0.001, and their median number of OPD visits was higher; 4.0 v 3.0 p < 0.001 (Table 2).
Viral Load Responses
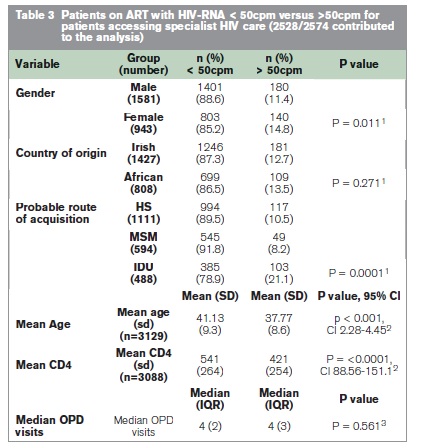
HIV RNA values were available on 2528/2574 (98.2%) of patients on ART; 2208/2528 (87.3%) had HIV viral load responses of < 50 copies per ml (cpm) and 2384/2528 (94.3%) < 500cpm. Those who were virally suppressed (defined as VL<50cpm) were older; 41.1 v 37.8 years, p < 0.001 and had a higher CD4 count 541 cells/mm3 v 421 cells/mm3, P<0.0001 (Table 3). For viral loads < 50cpm multi-variate analysis showed that only age remained significant with an odds ratio of 0.94(95% CI 0.93-0.95).
Antiretroviral Regimens
ART regimen was recorded for 2488/2574 (96.7%) of patients on treatment. 1065 (42.3%) and 1073 (42.9%) were on a nucleoside/nucleotide reverse transcriptase inhibitor backbone (NRTI) with a non-nucleoside reverse transcriptase inhibitor (NNRTI) or protease inhibitor (PI) regimen respectively.
Discussion
We present, for the first time, a descriptive profile of HIV-infected patients accessing care in the Republic of Ireland. These data describe a cohort of patients who are successfully accessing antiretroviral therapy. 80.4% of patients attending clinics are on ART and of these 87.3% have reported HIV RNA levels of < 50 cpm. However caution is needed as these data also highlight risk groups where barriers to treatment and compliance with treatment, reflected by viral load suppression, when started is an on- going issue; notably in younger patients and injecting drug users. Overall these data support the current model of specialist led regional HIV clinics in Ireland with additional resources being required for higher needs patients. 3254 patients were identified as accessing care showing a discrepancy with the number of new diagnoses ever reported to the HPSC since reporting began (6979). Notwithstanding the limitations of this study along with natural attrition due to reported deaths of 50510 and emigrations, there remain a large proportion of patients unaccounted for. This potentially highlights a group that may have been lost to follow up and are no longer linked to specialist care. This is also reported as a concern in other cohorts internationally, who report that 25%–44% of HIV-infected individuals are entirely lost to follow-up in many settings.11, 12 This study was a retrospective, cross sectional study relying on outpatient clinic databases and patient attendances to identify adults living with HIV. Patients who did not receive outpatient care, because they are not engaged in care or who only accessed inpatient care, were not included. There is a small possibility of duplicate data, however the author reviewed the final database to identify and remove same using the unique identifier of initials and date of birth for each individual. Further limitations include: the collection of potentially incomplete data due to the utilisation of multiple source documents; recall bias due the retrospective nature of the study and that the year of diagnosis and thus duration of diagnosis was not collected. Lastly the absence of mortality data during the 12-month period mean it is difficult to ascertain outcome data, despite the high ART use.
The data presented here are as a result of a valuable collaborative process between all 6 specialist HIV centres in Ireland and the HPSC. It is the first study of its kind in Ireland to estimate prevalence of HIV and despite its limitations will serve as a platform to initiate regular collation of these data. A crude national HIV diagnosed prevalence rate amongst 15-59 year olds is estimated at 1.09/1000 and in the Dublin area this rate reaches 2.25/1000. This study shows that Dublin is an area of high, diagnosed HIV prevalence and routine opt out testing for HIV in healthcare settings should be considered with the aim of improving timely diagnosis where HIV status is unknown.
Correspondence: H Tuite
Department of Infectious Diseases, Galway University Hospital, Newcastle Road, Galway
Email: [email protected]
Acknowledgements
Thanks to the following people for their help with this study: N Boyle, Galway University Hospital; V Treacy, M Moriarty, S Murphy, J Craig, St James’s Hospital; F Aherne, Cork University Hospital; D Redmond, P Hollywood, J Byrne, Beaumont Hospital; C Boyle, A Power, Mater Misericordiae Hospital; and A Macken, UCD HIV Molecular Research Group.
References
1. Donnell D, Baeten JM, Kiarie J, Thomas KK, Stevens W, Cohen CR, McIntyre J, Lingappa JR, Celum C. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. 2010 Jun 12;375:2092-8.
2. Dodd PJ, Garnett GP, Hallett TB. Examining the promise of HIV elimination by 'test and treat' in hyperendemic settings. Aids. [Research Support, Non-U.S. Gov't]. 2010 Mar 13;24:729-35.
3. HPA. Time to test for HIV: Expanding HIV testing in healthcare and community services in England: Health Protection Agency 2011 2011.
4. K O' Donnell, J Moran, D Igoe. HIV and AIDS in Ireland 2013. Health Protection Surveillance Centre; 2014 [cited2014 May]; Available from: http://www.hpsc.ie/A-Z/HIVSTIs/HIVandAIDS/SurveillanceReports/File,14651,en.pdf.
5. Health Protection Agency UK. Survey of Prevalent HIV Infections Diagnosed. 2011[cited 2012 November]; Available from: http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/HIV/AccessingHIVCare/hivsti_soph_SophidFAQ/.
6. BHIVA. UK National Guidelines for HIV Testing 2008. 2008 [cited 2012November]; Available from: http://www.bhiva.org/HIVTesting2008.aspx.
7. Palfreeman A, Fisher M, Ong E, Wardrope J, Stewart E, Castro-Sanchez E, Peto T, Rogstad K, Sheather J, Gazzard B, Pillay D, O’Brien J, Delpech V, Lowbury R, Fleet R, Azad Y, Lyall H, Hardie J, Adegbite G, Rooney G, Whitehead R. Testing for HIV: concise guidance. Clinical Medicine. [Practice Guideline]. 2009 Oct;9:471-6.
8. Sanders GD, Bayoumi AM, Sundaram V, Bilir SP, Neukermans CP, Rydzak CE, Douglass LR, Lazzeroni LC, Holodniy M, Owens DK. Cost-effectiveness of screening for HIV in the era of highly active antiretroviral therapy. N Engl J Med. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.]. 2005 Feb 10;352:570-85.
9. CSO CD207: Population by Single Year of Age, Sex, Province County or City and Census Year. Available from: http://www.cso.ie/px/pxeirestat/Statire/SelectVarVal/Define.asp?maintable=CD207&PLanguage=0.
10. Personal communication: Dr Kate O’ Donnell, Surveillance Scientist, HPSC. (November 2012)
11. Coleman S, Boehmer U, Kanaya F, Grasso C, Tan J, Bradford J. Retention challenges for a community-based HIV primary care clinic and implications for intervention. AIDS Patient Care STDS. [Research Support, U.S. Gov't, P.H.S.]. 2007 Sep;21:691-701.
12. Mocroft A, Kirk O, Aldins P, Chies A, Blaxhult A, Chentsova N, Vetter N, Dabis F, Gatell J, Lundgren JD. Loss to follow-up in an international, multicentre observational study. HIV Med. [Multicenter Study Research Support, Non-U.S. Gov't]. 2008 May;9:261-9.
