Introduction
Children under 10 years old accounted for half of the calls to the Poisons Information Centre in 2010.1 Studies have reported that poisoning accounts for up 0.28% of ED visits, with median age 24 months and paracetamol the most common substance ingested. Most cases of acute poisoning are accidental, benign and non-toxic.2-5 A prospective cohort study noted at least one incident of poisoning or suspected poisoning in 19% of children by age three.6 The aim of this study is to analyse accidental poisoning cases presenting to a tertiary paediatric hospital, to determine the most common substances implicated in these presentations and to compare the results with a similar study undertaken in the same institution ten years previously.7
Methods
This is a retrospective review of the Temple Street Children’s University Hospital (TS CUH) Emergency Department (ED) information management system (Symphony, Ascribe Ltd). This system is used to identify cases of accidental ingestion by discharge diagnosis. All episodes discharged from ED under ‘Toxicology, Accidental’ from the 1st of January 2010 until 31st of December 2011 were included. Demographic details, triage diagnosis, length of stay and outcome of episode were available directly from the system, while all other information was gathered from notes.
Results
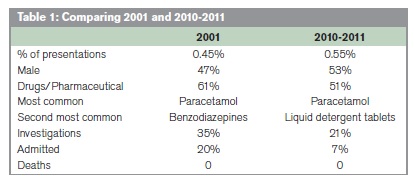
88623 attendances to TSCUH ED were recorded between 1st January 2010 and 31st December 2011. Of these, 478 (0.54%) were discharged with a discharge diagnosis under the heading of ‘toxicology’. 53.1% were male. Median age on presentation was 2 years and 5 months. The median length of stay in the ED was 2 hours and 37 minutes. The most common category of discharge diagnosis was ‘accidental drug poisoning’, accounting for 51.5% of presentations. Household products were responsible for 25% of presentations. The most common substance implicated was paracetamol (14%). Liquid detergent tablets were responsible for 9.2%. No investigations were performed in 79.3% of episodes. Paracetamol levels were performed at 4 hours post-ingestion in 4% of episodes, as ingestion was potentially over 150mg/kg as per guidelines. None of the paracetamol levels performed required treatment. Other toxicology tests were performed in 4.8% of episodes – including urine and serum toxicology for benzodiazepines, salicylates and other drugs. 93% of presentations required observation. In 4% of children the administration of activated charcoal by NG was recommended by Toxbase – including cases of recent benzodiazepine and tricyclic antidepressant ingestion. 3% of cases required other treatment: including drinking milk. There was evidence that Toxbase was consulted in 76.9% of the applicable cases, and the NPIC was contacted in 16.2%. 92% of episodes were discharged from ED – with review scheduled in 7.3% of cases. Of those admitted, 91% went to the ward and 9% to ICU.
Discussion
In 2001, a comparable study was conducted in the ED of TSH, when accidental ingestions accounted for 0.4% of presentations. The male:female ratio did not change significantly. Drugs and pharmaceutical products accounted for 61% of presentations in 2001 but only 51% in 2010-2011. Paracetamol was the most common substance accidentally ingested in both studies. The second most common substance ingested in our study was liquid detergent tablets, whereas these were not available in 2001 and the second most common substance ingested at that time was benzodiazepines. There were more investigations performed in the 2001 cohort – in 35% of presentations, while only 21% of presentations had investigations performed in our cohort. More of the 2001 cohort (20%) were admitted than this study (7%). The NPIC campaign in 2012 highlighted the need to educate parents and caregivers further on the hazards of household substances.
Paracetamol should be kept out of reach and in child-resistant containers. There were numerous cases of benzodiazepines loose in handbags, which should be kept in child-proof containers. Liquid detergent capsules, first manufactured in 2001, are an emerging threat and appear to be very accessible – potentially based on their easy-to-reach location in kitchens or utility rooms. Morbidity in accidental ingestions of liquid detergent capsules can be varied and severe, and involve the eyes, the upper gastrointestinal tract and the respiratory system.8-13 Reducing the accessibility of these hazards should include focusing on the provision of child-resistant packaging.
Correspondence: CM Moore,
Children’s University Hospital, Temple St, Dublin 1
Email: [email protected]
References
1. Poisons Information Centre of Ireland. Poisons Information Centre of Ireland Annual Report 2010. Dublin, 2011:9.
2. Fazen LE, Lovejoy FH, Crone RK. Acute Poisoning in a Children's Hospital: A 2-Year Experience. Pediatrics 1986;77:144-51.
3. Lamireau T, Llanas B, Kennedy A, Fayon M, Penouil F, Favarell-Garrigues J-C, Demarguez JL. Epidemiology of poisoning in children: a 7-year survey in a paediatric emergency care unit. Eur J Emerg Med 2002;9:9-14.
4. Mintegi S, Fernández A, Alustiza J, Canduela V, Mongil I, Caubet I, Clerigué N, Herranz M, Crespo E, Fanjul JL, Fernández P, Humayor J, Landa J, Muñoz JA,Lasarte JR, Núñez FJ, López J, Molina JC, Pérez A, Pou J, Sánchez CA, Vázquez P. Emergency Visits for Childhood Poisoning: A 2-Year Prospective Multicenter Survey in Spain. Pediatr Emerg Care 2006;22:334-38 doi: 10.1097
5. Sibert JR, Craft AW, Jackson RH. Child-resistant packaging and accidental child poisoning. Lancet 1977;310:289-90.
6. Beautrais AL, Fergusson DM, Shannon FT. Accidental poisoning in the first three years of life. Aust Paediatr J. 1981 Jun;17:104-9.
7. Sharif F, Khan RA, Keenan P. Poisoning in a paediatric hospital. Ir J Med Sci. 2003 Apr-Jun;172:78-80.
8. Forrester MB. Comparison of Pediatric Exposures to Concentrated "Pack" and Traditional Laundry Detergents. Pediatr Emerg Care 2013;29:482-86.
9. Horgan N, McLoone E, Lannigan B, Flitcroft I. Eye injuries in children: a new household risk. Lancet. 2005 Aug 13-19;366:547-8
10. Mathew RG, Kennedy K, Corbett MC. Eyes and alkalis: Wave of paediatric eye injuries from liquid detergent capsules: BMJ. 2010 Mar 2;340:c1186.
11. Celentano A, Sesana F, Settimi L, Milanesi G, Assisi F, Bissoli M, Borghini R, Della Puppa T, Dimasi V, Ferruzzi M, Moro P, Rebutti I, Travaglia A, Severgnini P, Georgatos J, Davanzo F. Severe respiratory and esophageal effects resulting from ingestion of unit dose liquid laundry detergents: A case report. Clin. Toxicol. 2013;51(4):311-11.
12. Williams H, Bateman DN, Thomas SH, Scott RA, Vale JA. Exposure to Liquid Detergent Capsules: A Study Undertaken by the UK National Poisons Information Service:. Clin Toxicol (Phila) 2012;59:776–80.
13. Fraser L, Wynne D, Clement WA, Davidson M, Kubba H. Liquid detergent capsule ingestion in children: an increasing trend. Arch Dis Child. 2012 Nov;97(11):1007. doi: 10.1136