|
|
|
|
|
|
|
|
Breffini Anglim,Amy O'Higgins,Niamh Daly,Maria Farren,MJ Turner
|
|
|
|
B Anglim, A O'Higgins, N Daly, M Farren, MJ Turner
Department of Obstetrics & Gynaecology, Coombe Women & Infant’s University Hospital, Cork St, Dublin 8
Abstract
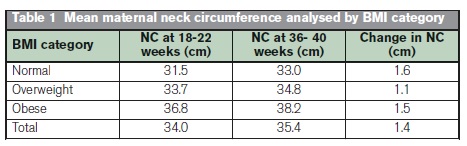
Obese women are more likely to require general anaesthesia for an obstetric intervention than non-obese. Difficult tracheal intubation and oxygen desaturation is more common in pregnancy. Failed tracheal intubation has been associated with an increase in neck circumference (NC). We studied the relationship between maternal obesity and NC as pregnancy advanced in women attending a standard antenatal clinic. Of the 96 women recruited, 13.5% were obese. The mean NC was 36.8cm (SD 1.9) in the obese women compared with 31.5cm (SD 1.6) in women with a normal BMI (p<0.001) at 18-22 weeks gestation. In the obese women it increased on average by 1.5cm by 36-40 weeks compared with an increase of 1.6 cm in women with a normal BMI. The antenatal measurement of NC is a simple, inexpensive tool that is potentially useful for screening obese women who may benefit from an antenatal anaesthetic assessment.
|
|
Introduction
Based on a Body Mass Index (BMI) > 29.9 kg/m2, maternal obesity is associated with an increase in pregnancy complications and interventions1,2. In particular, it is associated with interventions that may require general anaesthesia, such as caesarean section2,3. Outside pregnancy, difficult intubation is more common in obese than in lean patients. In a French study, a difficult intubation occurred in 15.5% (n=138) of patients with Class 2-3 obesity compared with 2-3% of lean patients (n=140)4. In another French study, difficult intubation occurred in 14.3% (n=10) of obese patients compared with 3.0% (n=2) in lean patients (p=0.03)5. The authors recommended that neck circumference (NC) should be measured preoperatively as a predictor of difficult intubation. There is a paucity of information about NC in pregnant women. The purpose of this longitudinal observational study was to examine the relationship between NC and maternal BMI as pregnancy advances.
Methods
Women who were attending a standard antenatal clinic were recruited at their convenience. Women had their weight and height measured in the first trimester before calculating the BMI. Clinical and sociodemographic details were recorded at the first antenatal visit after sonographic confirmation of an ongoing pregnancy. Women with a multiple pregnancy, women <18 years old and women who were unable to give consent were excluded. A single researcher (BA) then measured the neck circumference at the level of the thyroid cartilage with the head erect. This was carried at 18-22 weeks gestation, and repeat in the same population of women at 36-40 weeks gestation. The tape was held snug without compressing the skin.
Results
The patient characteristics are shown in Table 1. Of the 96 the mean age was 29.9 years (SD 5.71 (24.12346-35.60569)). The mean BMI was 25.4kg/m2 and 13.5% were obese based on a BMI > 29.9 kg/m2. The mean maternal NC analysed by BMI category is shown in Table 1. There were five (38%) women with a NC >39 cms in the obese women compared with 0% in the non-obese women (n=83) (p<0.001). Obese women had a greater NC than women with a normal BMI but the increase in NC as pregnancy advanced was similar. This indicates that a screening NC in early pregnancy could identify those obese women who are at a higher risk of a failed intubation.
Discussion
This observational study found that the mean NC was significantly higher in obese women and that in both obese and non-obese women it increased as pregnancy advanced. We suggest that before term, the obstetrician also measures the NC in all obese women. Outside pregnancy a NC>43cm is associated with a problematic intubation in about one in twenty cases5. Pregnancy is a unique state which causes physiological and anatomical changes that result in difficult airway. These changes are more pronounced in the pre-eclamptic woman, with higher rates of pre-eclampsia seen in obese women6-8. Given these physiological and anatomical changes, a smaller neck circumference than 43cm found to cause difficult intubation in non-pregnant women, is likely to cause difficulties. In an obese woman with an increased risk, skilled anaesthetic assistance and a wider range of equipment to facilitate intubation should be available4.
This study has strengths because BMI was calculated on measurement of weight and height which has been shown to be more reliable than self-reporting. We also have measured NC accurately at different time points during the pregnancy. A weakness of this pilot work is that the numbers were small and the recruitment was convenient and not consecutive. About one in six women booking for antenatal care in our Hospital is obese and they are a group who are at risk of an adverse outcome is increased if the patient requires intubation. The measurement of NC is a simple non-expensive screening tool which should be evaluated further in a larger prospective study.
Correspondence: B Anglim
Department of Obstetrics & Gynaecology, Coombe Women & Infant’s University Hospital, Cork St, Dublin 8
Email: [email protected]
References
1. Farah N, Maher N, Barry S, Kennelly M, Stuart B, Turner MJ. 2009. Maternal morbid obesity and obstetric outcomes. Obesity Facts 2: 352-4.
2. O’Dwyer V, Farah N, Fattah C, O’Connor N, Kennelly MM, Turner MJ. 2003. The risk of caesarean section in obese women analysed by parity. European Journal of Obstetrics and Gynecology and Reproductive Biology 158: 28-32.
3. Tan T, Sia ST. 2011. Anesthesia Considerations in the Obese Gravida. Seminars in Perinatology 35: 350-355.
4. Juvin P, Lavaut E, Dupont H, Lefevre P, Demetriou M, Dumoulin JL, Desmonts JM. 2003. Difficult tracheal intubation is more common in obese than in lean patients. Anesthesia and Analgesia 97: 595-600
5. Gonzalez H, Minville V, Delanoue K, Mazerolles M, Concina D, Fourcade O. 2008. The importance of increased neck circumference to intubation difficulties in obese patients. Anesthesia and Analgesia 106: 1132-6
6. Norwitz ER, Robinson JN, Malone FD: Pregnancy-induced physiologic alterations. In: Critical Care Obstetrics. Fourth Edition. Dildy GA, Belfort MA, Saade GR, et al. (Eds). Malden, MA: Blackwell Science, 2004, 19–42
7. Brimacombe J. 1992. Acute pharyngolaryngealoedema and pre-eclamptic toxaemia. Anaesthetic Intensive Care 20: 97–98
8. Heidemann B, McClure J. 2003. Changes in maternal physiology during pregnancy. British Journal of Anaesthesia 3: 65-68
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|