Introduction
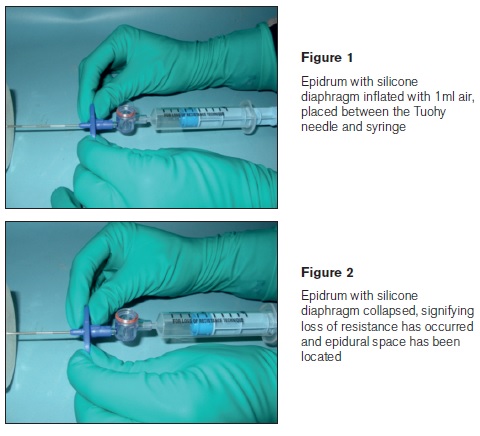
Neuraxial analgesia is widely recognised as the most effective form of pain relief during labour.1 Whilst generally safe, it has potential complications. After inadequate analgesia, the most common one is Accidental Dural Puncture (ADP) with a quoted incidence of 0.19% - 3.6% of obstetric epidurals.2 Following ADP, the incidence of Post Dural Puncture Headache (PDPH) is quoted as anything from 50% to 81%.3,4 It is often severe and incapacitating, prolonging hospital stay, and can have a detrimental effect on maternal-infant interaction.5 Identification of the epidural space is crucial to the provision of epidural analgesia. Over the years various methods have been described, such as Loss of Resistance (LOR) to air or 0.9% Saline and the ‘hanging drop’ technique.6 Since the development of modern LOR syringes, the LOR technique has become the technique of choice. A survey of epidural technique among obstetric anaesthetists in 2001 showed that up to 70% of respondents were using a LOR to Saline (LORS) technique.7 The Epidrum (Exmoor Innovations Ltd. Taunton, Uk) is an optimal, constant, low pressure air operated LOR device developed to facilitate identification of the epidural space. It comprises of a plastic drum like cylinder with a thin silicone diaphragm. When placed between the Tuohy needle and syringe the user injects the Epidrum with 1ml of air to expand the diaphragm in a balloon like manner. This allows the operator to use two hands to control the epidural needle whilst providing continuous low pressure at the needle tip. After careful advancement of the needle, sudden collapse of the diaphragm signifies LOR and identification of the epidural space. It has been proposed that using the Epidrum may improve identification of the epidural space, reduce associated morbidity and provide teaching opportunities, as observers can also identify the moment of LOR. The aim of our pilot study was to determine if using the Epidrum improves success and reduces morbidity when compared to LORS technique.
Methods
After ethical approval and written informed consent, 300 parturients requesting epidural analgesia for labour, were enrolled in our study. Patients younger than 18 or those unable to give informed consent were excluded. The 300 subjects were randomised into two groups using computer generated numbers. One group (Epidrum group) received epidural analgesia using the Epidrum and the other group (Control group) received epidural analgesia using standardised LORS technique. All epidurals were performed by seven trainee anaesthetists rotating through the hospital during the period of the study. The experience of our operators in anaesthesia ranged from 1.5 to 8 years. All the trainee anaesthetists who participated in the study were trained in using the Epidrum device (via a simulated LOR device provided by Exmoor Innovations Ltd.) prior to using it on patients. All epidurals were carried out with subjects in the sitting position, using an 18 gauge Tuohy needle with the bevel facing cephalad. After location of the epidural space, the epidural catheter was advanced 4 cm into the epidural space in all subjects. A standardised test dose and maintenance infusion was used in all subjects. If the trainee failed to site the epidural after three attempts, a second anaesthetist was called to carry out the procedure,using their technique of choice.
We recorded the following variables in the labour ward: subject demographics, anaesthetic experience of the operator in years, dural puncture, number of attempts taken to site epidural, failure (defined as being unable to site the epidural catheter after three attempts) to site epidural requiring a second operator, and failure of epidural analgesia (defined as failure to obtain a sensory block after initial local anaesthetic loading dose, resulting in the epidural catheter being re-sited). The subjects were followed up in the next 24-48 hours by an anaesthetist who was blinded as to group allocation in order to detect the occurrence of PDPH in the first 48 hours. The performance of epidural blood patches (EBP) on any of the subjects was also recorded. In addition the subjects were followed up with a telephone interview at 6 weeks to ensure we had not missed any atypical delayed onset PDPH. Data were compared using an independent samples t-test for continuous measures. For categorical measures Pearson’s chi-squared test was used. A Fisher’s exact test was used to compare the data in variables were the expected frequency was less than 5 in greater than 25% of the subjects; need for second operator, accidental dural puncture, failure of analgesia, PDPH and EBP. All comparisons were made with a level of significance of 0.05.
Results
There were no significant differences between the two groups for age, height, weight, BMI, parity or anaesthetic experience (Table 1). There were no significant differences between techniques except for failure to site the epidural requiring a second operator. In 9 out of 150 epidurals (6%) in the Epidrum group a second anaesthetist was required to site it, compared to none in the Control group (P=0.003) (Table2). There were four accidental dural punctures in the Epidrum group and none in the Control group (P=0.060). Two of these subjects suffered from a PDPH as a result. One subject was managed conservatively and the other received an epidural blood patch. In the Epidrum group two out of 150 epidurals were re-sited, versus three out of 150 epidurals in the control group (P=1.000).
Discussion
Our pilot study showed that use of Epidrum to site epidurals was equivalent to LORS,except for failure to site the initial epidural where LORS was superior. It is the first study using the Epidrum to look specifically at morbidity as a primary outcome. It is also the largest study so far comparing Epidrum8,9 to standard LOR techniques. The principle aim of our pilot study was to estimate population rates of adverse events in each group. Therefore the number of participants (150 per group) was selected not to sufficiently power any hypothesis tests, but to attempt to observe sufficient numbers of events to adequately estimate the rates, given the time and resources available. We note that 150 individuals undergoing a procedure with a 3.6% adverse event rate (as per ADP) would be expected to return 5.4 events on average, or 4 or more events with 80% probability, giving tight 95% confidence intervals for the rate of approximately +/- 2 to 2.5 percentage points. By adverse event we mean ADP, PDPH and EBPs. The published adverse event ranges are broad (0.2%to 3.6% for ADP, 0.1% to 2.9% for PDPH), but centred around a 1-2% rate. Powering a study to detect even a 1 or 2 percentage point shift between groups would require a sample with at least twice as many participants as the present study, ranging up to several thousand participants per group. This was not feasible in the present study, nor justifiable given the uncertainty surrounding the rates of adverse events in this population, and with each of the devices. We hope to have addressed some of this uncertainty with the present study.
We additionally note that the actual power for a comparison of binary event rates is critically dependent on the actual observed rate, an unknown until the study is completed. In our case we observed an unexpectedly low rate of ADP and PDPH (0%) in one group, which improved our power considerably, and is mostly likely responsible for the "nearly significant" p-values reported. One confounding factor in our study is that the mean experience of our trainees was high, 5.54 years and 5.95 years in the Control and Epidrum groups respectively. There may also have been individual operator bias. Some of our investigators enthusiastically adopted the new device whilst others preferred their usual LOR technique. The small number of investigators in the study (n=7) may have provided an opportunity for individual bias to skew the results in favour of one technique over another. As such, it would seem prudent when designing a future randomised controlled trial to engage anaesthetic operators of a similar experience, preferably novice as in the pilot study we found experienced operators were less enamoured with the new device.
Our results differ somewhat from two previous studies carried out comparing the Epidrum to standard LOR techniques.8,9 Both these studies found the Epidrum to be superior to conventional LOR techniques, however they focused more on the time taken to carry out the procedure and ease of use, while our study looked primarily at morbidity and clinical endpoints. While our results did not show the Epidrum to offer any real advantage to LORS for siting epidurals, it may have a useful role to play in the teaching of the epidural procedure. It is often difficult for an anaesthetist teaching a trainee to determine whether there is a true loss of resistance simply by observing the procedure. If used correctly the Epidrum provides a very obvious visual signal that the epidural space has been reached, thus removing operator and observer subjectivity. In conclusion, the results of our pilot study do not suggest that using Epidrum compared to the standard LORS technique improves success or reduces morbidity associated with labour epidurals. All comparisons are from within our study.
Correspondence: M Deighan
National Maternity Hospital, Holles St, Dublin 2
Email: [email protected]
Acknowledgements
Thanks Exmoor Innovations Ltd. Taunton, and R Segurado and CSTAR School of Public Health, Physiotherapy and Population Science, University College Dublin, for their help with this study.
References
1. Van de Velde M. Modern neuraxial labor analgesia: options for initiation, maintenance and drug selection. Rev Esp Anestesiol Reanim. 2009; 56: 546-61.
2. Hollister N, Todd C, Ball S, Thorp-Jones D, Coghill J. Minimising the risk of accidental dural puncture with epidural analgesia for labour: a retrospective review of risk factors. Int J Obstet Anesth. 2012; 21: 236-41.
3. Lybecker H, Djernes M, Schmidt JF. Post dural puncture headache (PDPH): Onset, duration, severity, and associated symptoms. An analysis of 75 consecutive patients with PDPH. Acta Anaesthesiol Scand. 1995; 39: 605-12.
4. Paech M, Banks S, Gurrin L. An audit of accidental dural puncture during epidural insertion of a Tuohy needle in obstetric patients. Int J Obstet Anesth. 2001; 10: 162-7.
5. Van de Velde M, Schepers R, Berends N,Vandermeersch E, De Buck F. Ten years of experience with accidental dural puncture and post-dural puncture headache in a tertiary obstetric anaesthesia department. Int J Obstet Anesth. 2009; 17: 329-335.
6. Van de Velde M. Identification of the epidural space: Stop using the loss of resistance to air technique! Acta Anaesthiol Belg. 2006; 57: 51-4.
7. Cowan CM, Moore EW. A survey of epidural technique and accidental dural puncture rates among obstetric anaesthetists. Int J Obstet Anesth. 2001; 10: 11-16.
8. Sawada A, Kii N, Yoshikawa Y, Yamakage M. Epidrum: A new device to identify the epidural space with an epidural Tuohy needle. J Anesth. 2012; 26: 292-5.
9. Kim SW, Kim YM, Kim SH, Chung MH, Choi YR, Choi EM. Comparison of loss of resistance technique between Epidrum and conventional method for identifying the epidural space. Korean J Anesthesiol. 2012;62: 322-6.
