Introduction
Smoking is currently the largest avoidable cause of premature mortality and disability in the world, and helping smokers to quit smoking is the most cost-effective intervention available1. In Ireland, it is estimated that 36,000 hospital discharges per year are attributable to smoking2. Hospital admission is an opportunity to identify smokers and offer help to stop smoking. Clinical guidelines recommend the ascertainment of smoking status and the delivery of smoking cessation interventions in all health consultations3. SLÁN 2007 reported that almost half (48%) of adults were current or former smokers4. Recent figures from the National Tobacco Control Office report that the prevalence of cigarette smoking in Ireland is currently at 21.7%5.
International literature on the prevalence of current smoking among hospital patients varies widely: UK studies report that 13% of hospital patients were current smokers;6 studies from the United States and Brazil report that between 15% and 25% of hospital inpatients are current smokers7-10; however, additional studies from Australia, Italy and San Francisco in the United States estimate that as many as 40% of hospital patients may be active smokers11-15. In Ireland, St Vincent’s University Hospital in Dublin, has published widely on smoking prevalence in their hospital population16,17. In 2010, they reported that 18% of inpatients were current smokers, down from a rate of 22.7% in 200617. In 2012, a study in Beaumont Hospital reported that 21% of a sample of their inpatients was current smokers, with 61% of them reporting that they had been asked by a healthcare professional about smoking in the previous twelve months18. In 2007, a Health Service Executive (HSE) commissioned National Consumer Satisfaction Study reported that 29% of respondents were current smokers, and that 49% of them had received information about stopping smoking, mostly leaflets19. The aim of this study was to determine the proportion of inpatient hospital discharges from acute hospitals in Ireland, who had tobacco use recorded as a diagnosis on their medical record, as reported on the Hospital In-Patient Enquiry (HIPE) System.
Methods
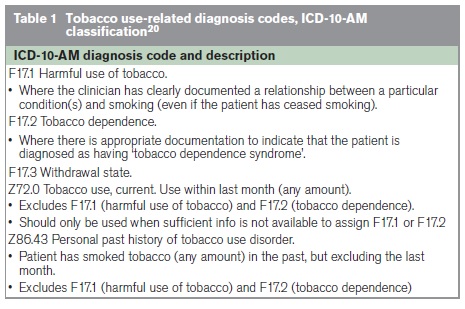
Data for this study were extracted from the Hospital In-Patient Enquiry (HIPE) system via Health Atlas Ireland (HAI). HAI is an open source application which enables web-based mapping of health-related data on a national basis. All inpatient discharges (excluding maternity, HIPE code admission type 6) from acute hospitals in the Republic of Ireland, aged 18 years and over, with any diagnosis of tobacco use were extracted for the years 2005-2011. Tobacco use was defined as per Table 1. Results are presented by year of hospital discharge, age and gender and consultant specialty. Using HAI, additional analysis was carried out on those discharges aged 35 years and older, who had a principal diagnosis of a smoking-related condition as defined by Callum & White from the London Health Observatory21 to determine the level of recording of tobacco use among these groups.
Results
The Recording of Tobacco Use on HIPE, 2005-2011
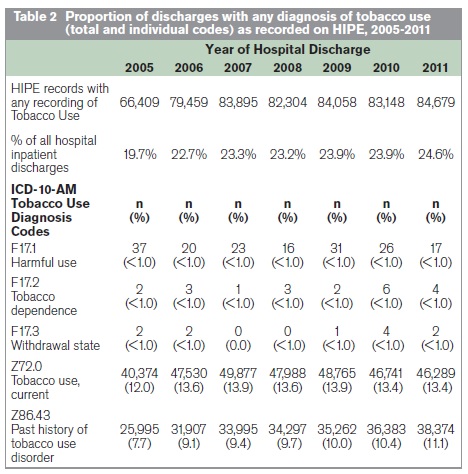
In 2011, 24.6% (n=84,679) of inpatient discharges had a recording of tobacco use (current or past) on their HIPE record. This compares to 19.7% (n=66,409) in 2005. Looking at the individual codes as detailed in Table 2, the most commonly recorded diagnosis codes were Z72.0 current tobacco use and Z86.43 past history of tobacco use disorder. Few recorded the F17.1, F17.2 or F17.3 diagnosis codes. In 2011, 13.4% of inpatients had a diagnosis of Z72.0 current tobacco use and 11.1% had a diagnosis of Z86.43 past history of tobacco use. This compares to 12.0% (current) and 7.7% (ex-smokers) in 2005.
Profile of the Discharges with a Recording of Tobacco Use as Reported on HIPE, 2011
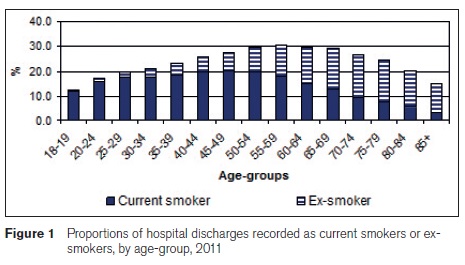
Figure 1 details the proportion of hospital discharges recorded as being current smokers (Z72.0) or ex-smokers (Z86.43), by age-group in 2011. The highest level of recording of any tobacco use was among those aged 55-59 years (30.6%), with the lowest level among those aged 18-19 years (12.6%). Looking at current smokers, the highest proportion were among discharges aged 45-49 years (20.2%), after which the levels decreased with increasing age. The proportion of ex-smokers increased with increasing age, with the highest proportion of ex-smokers among those aged 70-74 years (17.3%). The majority (73%) of ex-smokers were aged 60+ years.
Almost 30% (28.6%) of male discharges had a recording of tobacco use compared to 20% of females. In 2011, similar proportions of male and female discharges were recorded as being current smokers (male:14.7%, female:12.2%); however, almost twice as many male discharges were ex-smokers (13.9%) compared to females (8.3%). By consultant specialty, almost 30% (28.5%) of medical discharges had a recording of tobacco use compared to 19.7% of other discharges. In 2011, 14.7% of medical discharges were recorded as being current smokers and 13.8% were ex-smokers, compared to 11.8% (current) and 7.9% (ex) of other discharges.
Discharges aged 35+ Years with smoking-related diseases/conditions
Figure 2 details the level of recording of tobacco use among discharges aged 35 years and over, with a principal diagnosis of a smoking-related condition as defined by Callum & White 21 for 2011. The highest level of recording of tobacco use was among those with a principal diagnosis of cancer of the larynx (58.6%), followed by chronic airway obstruction (55.4%) and cancer of the trachea, lung and bronchus (55.3%). The lowest rate was among those with cataracts (3.8%).
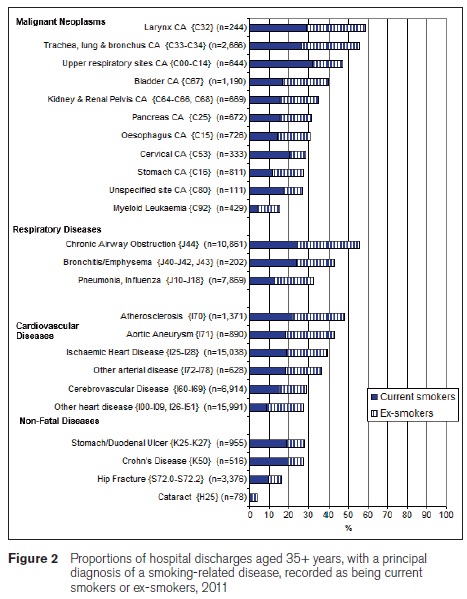
Patients with a principal diagnosis of cancer of the upper respiratory sites (32.1%), cancer of the larynx (29.1%) and cancer of the trachea, lung and bronchus (26.6%) were most likely to be current smokers, while, those with a principal diagnosis of chronic airway obstruction (30.6%), cancer of the larynx (29.5%) and cancer of the trachea, lung and bronchus (28.7%) were most likely to be ex-smokers.
Discussion
Hospital admissions are an opportunity to identify smokers and to offer help to enable them to quit. Clinical guidelines recommend the ascertainment of smoking status and the delivery of smoking cessation interventions in all health consultations3. The aim of this study was to determine the proportion of inpatients with a recording of tobacco use on their medical record, as reported on HIPE. This study reports that a quarter (24.6%) of inpatients had any recording of tobacco use on their medical record. SLÁN 2007 reported that 48% of adults have smoked at some stage in their lives4. Looking at type, 13.4% of inpatients were current smokers, defined as having smoked in the last month, while 11.1% were past smokers, defined as having smoked in the past, but excluding the last month. The National Tobacco Control Office reports that 21.7% of the Irish population are current smokers, defined as smoking at least one cigarette per week5. This data would suggest that there is an under-reporting of tobacco use (current and past) among these hospital inpatients.
HIPE is the only data source for this report, and is the only source of morbidity data available nationally for acute hospital services in Ireland. It has high quality controls and is managed by the Healthcare Pricing Office. There are limitations to this study. The data source itself (HIPE) records episodes of care and does not allow for the tracking or linking of individual patients through the hospital system. Due to the lack of unique identifiers, patients may be admitted to hospital more than once in any given period with the same or different diagnoses, or admitted to different hospitals and therefore given a different medical record number. However, we feel that these limitations will not impact greatly on our study, as the overall aim was to report on the level of recording of patients’ history of tobacco use on medical records during their hospital admission. Most of this report considered the diagnostic codes Z72.0 and Z86.43 as 99.9% of the data concerned these two codes, with less than 1% relating to the F17.1, F17.2 and F17.3 codes (see Table 1). A review of these codes’ definitions would indicate that in most cases, the F17.1 and F17.2 diagnoses codes are the more appropriate codes. However, they can only be used when a relationship between the condition and smoking is documented; as a result, the codes Z72.0 and Z86.43 are only to be used where insufficient information is available. However, as our analyses displays, Z72.0 and Z86.43 are the ‘default’ codes used in most cases. This may indicate a lack of information by medical personnel in the medical record, thus preventing the coder from using the most appropriate code as per coding guidelines. Either way, there should be an emphasis placed on using the most appropriate codes for the purposes of quality improvement. The level of under-reporting of tobacco use among patients in Irish hospitals is difficult to determine due to the fact that we cannot quantify the numbers who ‘never-smoked’; there are no codes in the WHO ICD classification for ‘never smoked’. Therefore, we cannot distinguish between the proportions of those who never smoked, and an under-reporting of tobacco use on HIPE.
The report ‘Tobacco in London: The Preventable Burden’ produced by the London Health Observatory21 details a methodology which allows for the estimation of the smoking-attributable proportion of hospital admissions for a number of smoking-related conditions, as listed in Figure 2. In our analysis, in particular, many cancers and diseases of the respiratory system had low proportions of inpatients with a recording of tobacco use, where a high proportion of these conditions are estimated to be smoking-related. For example, it is estimated that 84% of cancers of the trachea, lung and bronchus are smoking-related, yet just 55% of inpatients with a diagnosis of cancer of the trachea, lung and bronchus in this study had a recording of any tobacco use on their medical record. Similarly, just 43% of those with a diagnosis of bronchitis/emphysema had a recording of any tobacco use, where it is estimated that 86% of cases of bronchitis/emphysema are smoking-related. And, while hospitals should ascertain the smoking status of all inpatients on hospital admission, those with smoking-related conditions should be a particular focus.
Continued efforts should be made to improve the quality of the coding of tobacco use on HIPE, by the medical personnel in documenting a relationship between the patients’ condition and smoking, thus enabling the coders to use the most appropriate codes as per coding guidelines. Smoking is currently the largest avoidable cause of premature mortality and disability in the world, and helping smokers to quit is the most cost-effective intervention. However, unless these patients are identified on occasions such as a hospital admission, they may not receive the necessary treatment and support to help them stop smoking. Efforts should be made to ensure that smoking status of all patients is ascertained at all health encounters as recommended by international clinical guidelines, and in particular patients with a smoking-related condition.
Correspondence: A Sheridan
Department of Public Health, HSE Dublin North East, Railway St, Navan, Co Meath
Email: [email protected]
Acknowledgements
The Hospital In-Patient Enquiry system (HIPE) provided by The Healthcare Pricing Office and the web based facilities of Health Atlas Ireland.
References
1. Tobacco. Fact Sheet Number 339. World Health Organization. July 2013.
2. Sheridan A, Howell F. Smoking-related discharges, bed days and costs in acute hospitals, 2008-2010. Health Service Executive, Navan, Co. Meath. 2013.
3. National Institute for Health and Care Excellence. Brief Interventions and referral for smoking cessation in primary care and other settings. London. 2006.
4. Brugha R, Tully N, Dicker P, Shelley E, Ward M, McGee H. (2009). SLAN 2007: Survey of Lifestyle, Attitudes and Nutrition in Ireland. Smoking Patterns in Ireland: Implications for policy and services, Department of Health and Children. Dublin: The Stationery Office.
5. National Tobacco Control Office. Cigarette Smoking Trends in Ireland. Health Service Executive, Dublin. 2013.
6. Murray R, Leonardi-Bee J, Marsh J, Jayes L, Britton J. Smoking status ascertainment and interventions in acute medical patients. Clinical Medicine Vol 12, No 1: 59-62.
7. Regan S, Viana JC, Reyen M, Rigotti NA. Prevalence and Predictors of Smoking by Inpatients During a Hospital Stay. Archives of Internal Medicine, 172: 1670-74.
8. Oliveira MV, Oliveira TR, Pereira CA, Bonfim AV et al. Smoking among hospitalised patients in a general hospital. J Bras Pneumol. 34: 936-41.
9. Figlie NB, Oillon SC, Dunn J, Laranjeira R. The frequency of smoking and problem drinking among general hospital inpatients in Brazil – using the AUDIT and Fagerström questionnaires. Sao Paulo Medical Journal. 118: 139-43.
10. Barreto RB, Pincelli MP, Steinwandter R, Silva AP, Manes J, Steidle LJ. Smoking among patients hospitalized at a university hospital in the south of Brazil: prevalence, degree of nicotine dependence, and motivational stage of change. J Bras Pneumol. 38: 72-80.
11. Bittoun R, McMahon M, Bryant DH. Smoking in hospitalised patients. Addiction Behaviour. 16: 79-81.
12. Peach HG. Obesity, smoking and hazardous drinking among men admitted to the surgical wards of a regional hospital. Australian Journal of Rural Health 10: 273-7.
13. Benowitz NL, Schultz KE, Haller CA, Wu AH, Dains KM, Jacob P 3rd. Prevalence of smoking assessed biochemically in an urban public hospital: a rationale for routine cotinine screening. American Journal of Epidemiology 170: 885-91.
14. Vernon JD, Crane LA, Prochazka AV, Fairclough D, MacKenzie TD. Smokers hospitalized in an urban, public hospital: addiction, stages of change and self-efficacy. Preventative Medicine 28: 488-95.
15. D’Avanzo B, La Vecchia C, Karsouyanni K, Negri E, Trichopoulos D. Reliability of information on cigarette smoking and beverage consumption provided by hospital controls. Epidemiology 7: 312-5.
16. Fitzpatrick P, Gilroy I, Doherty K, Corradino D, Daly L, Clarke A, Kelleher CC. Implementation of a campus-wide Irish hospital smoking ban in 2009: prevalence and attitudinal trends among staff and patients in lead up. Health Promotion International 24: 211-22.
17. Fitzpatrick F, Gilroy I, Doherty K, Clarke A, Comerford D, Daly L, Kelleher C. Smoke free hospital campus: Strong positive shift in attitudes post implementation but paradox in nursing and medical attitudes. Clinical Health Promotion 2: 12-8.
18. Bartels C, AbuHaliga ARY, McGee H, Morgan K, McElvaney NG, Doyle F. A survey of the prevalence of smoking and smoking cessation advice received by inpatients in a large teaching hospital in Ireland. Irish Journal of Medical Science.
19. Insight 07. Health and Social Services in Ireland – a survey of consumer satisfaction. Health Service Executive. Dublin. 2008.
20. Tabular List of Diseases. Volume 1 of the International Statistical Classification of Diseases & Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM). National Centre for Classification in Health, Australia. 2004.
21. Callum C, White P. Tobacco in London: The preventable Burden. The London Health Observatory. 2004.
