Abstract
Accurate data on primary care activity is key to health services planning and reconfiguration. Official data estimate general practice adult consultation rates to be 3.2 visits annually, based on patient self reports. We aim to estimate the consultation rate using practice based data and compare this to official estimates. We interrogated six general practices’ information systems and estimated consultation rates based on practice, telephone, domiciliary and out of hours consultations by patients aged 18 years or older. The study population (20,706 patients) was representative of the national population in terms of age and GMS status. The mean consultation rate was 5.17, though this was higher among GMS-eligible patients and among older age groups. Estimates of consultation rates derived from practice based data are likely to be higher than that derived from other approaches. Using multiple sources of data will enhance accuracy of workload estimates and this will benefit service planning.
Introduction
General practice and primary care are key to the reconfiguration of health services in Ireland. Accurate data on workload, morbidity and health service utilisation is necessary. Though official data estimated Irish general practice consultation rates to be 3.2 visits annually in 2010 (2.8 visits in 2007), this estimate is based on patient self reports alone and does not consider data contained in general practice based information systems. There is an increasing recognition that such health information systems have key role in this respect. This paper aims to estimate the consultation rate at a sample of Irish general practices using general practice information systems.
The method of funding Irish general practice is unique by international comparisons. Forty-three per cent of the population access free GP care through Ireland’s General Medical Services (GMS) scheme1. Irish GPs, with a few exceptions, are paid a ‘capitation fee’ according to the patient’s age and sex to provide 24 hour care for these patients2. ‘Full’ GMS eligibility is determined predominantly on the basis of low income with patients aged 70 and older being allowed a much higher income threshold. About 6% GMS cards are ‘GP Visit Cards’ (GPVCs) which allow patients free access to their GP without the benefit of free medications and access to the other community services. The GPVC is granted on the basis of the medical card income threshold plus 50% after certain living expenses are taken into account. In addition, a small proportion of the population are granted discretionary medical cards on the basis of experiencing ‘undue hardship. Therefore 57% of the population pay for general practice care though may be entitled to recoup a portion, depending on the extent of private health insurance. All GMS patients are registered with a GP. There is no national patient identifier and also no mandatory registration for private patients. The average adult standard consultation fee was €51 in 20103.
Official Irish adult patient GP Consultation rates are derived from the 2007 and 2010 National Quarterly Household Survey (NQHS)4,5. These estimates are based on recollection of consultations by patients over the previous 12 months which is at odds with the methodology used by ‘European Health Interview Survey’ which asked interviewees to report their doctor visits during the previous four weeks6. The 2007 and 2010 CSO survey methodology produces much lower attendance rates than several other estimates of consultation rate, including: CSO 2001 data which was based on recollection of consultations over the previous two weeks7; ‘Fee-per-item’ contract GP attendance rates based on administrative records and published annually by Ireland’s ‘Primary Care Reimbursement Service’2,8-11; and ‘QRESEARCH’ audit of 4.3 million patients involving 21.7 million clinical consultations in the UK12. In addition, these recent reports estimating GP consultation rate imply that consultation rates among GMS-eligible patients are similar for both younger and older patients which is again at odds with national and international evidence12-14. Therefore this paper aims to determine if General Practice consultation rates among Irish adults are as low suggested by this recent official data. A secondary objective was to explore if age and GMS status affect consultation rates.
Methods
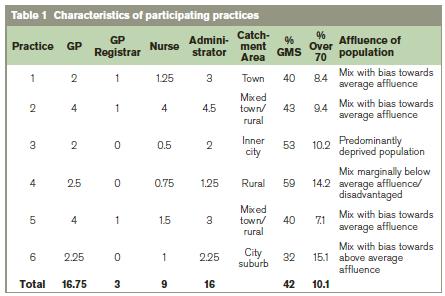
We estimated annual adult consultation rates at six general practices, purposefully selected based on interest in the topic under study and to be reflective of General Practice in Ireland15. Participating practices had a full complement of nursing and administrative staff and were located in all four of Ireland’s Health Service Executive (HSE) regions. Characteristics of participating practices (i.e. location, staffing, local area deprivation and practice demographics) are described in Table 1. The study period was the 12 months from 23/10/12 to 22/10/13. We adopted the same definition of consultation as that used by the ‘QRESEARCH’ audit of clinical consultations in the UK12 and the CSO NQHS, i.e. ‘direct contact between a clinician and patient either in the surgery, in the patients’ house or on the telephone’. Telephone contacts involving discussion of results, request for notes or a prescription were not considered as consultations. Clinic contacts at all six participating practices registered for inclusion as a consultation when a patient appointment coincided with a consultation note in the same patient’s record on the same day. Estimates of out of hours contacts and telephone consultations were based on records maintained at one practice and this figure was extrapolated to all six practices.
Calculation of the number of GMS patients was taken from each practice’s GMS list on the 01/04/2013. We estimated the number of ‘private’ patients in each practice from the number of unique private patient attendances during the 12 month study period and dividing by 0.7 (derived from 2010 CSO NQHS data which estimated that 70% of non-GMS patients attended their GP in the previous 12 months). Data at each practice was collected by a GP Principal at that practice, anonymised and only anonymised, aggregate data was reviewed / analysed by the principal investigator (WB).
Results
At participating practices, there was a total combined patient population of 27,080 in the six practices of whom 20,706 were aged 18 years or older. Whole time equivalent staff was estimated as 16.75 GPs, three GP registrars, nine practice nurses and 16 administrative staff. Characteristics of the study population were comparable to both Ireland’s national population and the national population of GMS-eligible patients (see Figure 1).
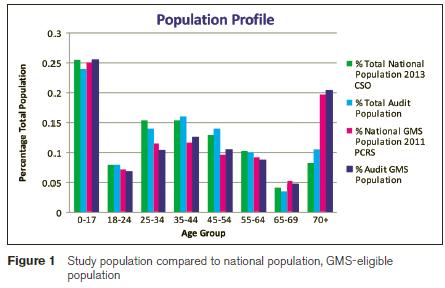
11,428 (42 % of total population) were GMS-eligible, which is comparable to the national reports1. We estimated the total population of ‘private patients to be 15,652. Of the GMS eligible population, 19.6% was aged over 69 which is similar to national population8. 10.1% of the total population (including children) were aged over 69 years which is a slightly higher percentage of over 69 year olds than the national population proportion of 8.2% according to the 2013 CSO projections. 23.5% of our population were under the age of 18 years old compared to 25.5% of the national population20. The consultation rate among all adult patients was 5.17; 7.72 among GMS-eligible patients and 3.35 among ‘private’ patients. GMS patients under the age of 70 attended 7.01 times per annum and 70s and those older attended 9.69 times per annum.
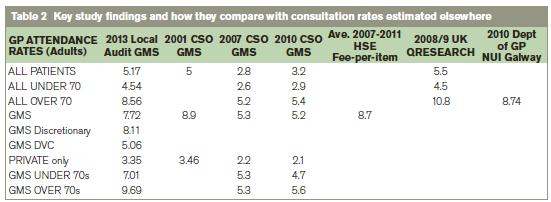
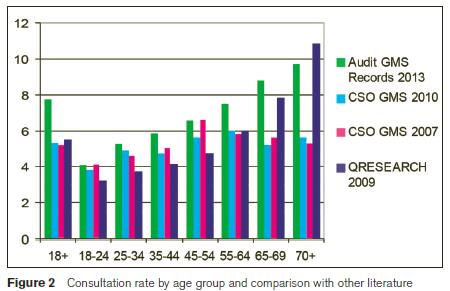
Almost all patients who had GPVCs or ‘Discretionary’ GMS cards were aged under 70. Consultation rate among patients with ‘Discretionary’ GMS cards was 8.11; this was higher than the consultation rate among all GMS patients aged under 70 (7.01) and patients with GPVCs (5.06). Compared to the 2007 and 2010 CSO surveys, the consultation rates we observed were higher among all age groups and medical card status. Older patients exhibit an increasing attendance rate, which would not be obvious in the CSO data (see Table 2).
Discussion
This cross sectional study of 20,706 adult patients at six general practices estimates a mean annual consultation rate of 5.17 in Irish general practice, with higher rates observed among GMS-eligible and older patients. Our findings suggest consultation rates in Irish general practice are higher than that estimated using other approaches, especially the 2007 and 2010 CSO data4,5. Other approaches that involve asking patients to report health service utilisation over a shorter period and that report data from clinical records would appear to provide higher, possibly more accurate, estimates of consultation rates7,12-14. In particular, our findings and especially that consultation rates are higher in older age groups, are consistent with those of Hippisley Cox12. Our data also mirrors a recent review of 427 patients (aged >55) attending General Practice over a 12-month period which reported a mean of 8.0 discrete clinical encounters, predominantly for respiratory conditions13. The most marked variance between our findings and the 2007 and 2010 CSO data involves older, GMS eligible patients – the groups with higher consultation rates. While the reasons for this are complex, relying on patients to report the number of visits over a longer time period is likely to under-estimate activity. That there was little variance between our study and the 2001 CSO data, in which patients were asked to report their medical contacts over the previous two weeks, would support this hypothesis.
The introduction of free primary care, by expansion and reconfiguration of the GMS system and the introduction of universal health insurance is a stated policy objective in Ireland16. Our findings suggest this policy will have considerable workload implications. Previous research in Ireland indicated that when older patients become eligible for free primary care / GMS services, they are exposed to more screening and general practice activity even after controlling for a variety of individual and household socio-economic and health status characteristics17. Furthermore, Nolan recently estimated 1.5-1.8 additional GP visits per person would result from the introduction of universal primary care an estimate that is consistent with our findings18.
Extrapolating our findings to a national population of 4.59 million (2013 CSO), suggests approximately 24 million consultations occur in general practice annually (15.4 million GMS consultations and 8.8 million private consultations). Were private patients to attend at the same rate as GPVC patients, then one might anticipate an increase in general practice workload of 4.4 million consultations per year, which is well in excess of the figures currently used in planning of Universal Primary Care19. The planned introduction of a national chronic disease management program would further inflate this figure.
While our study population is large and reflective of the national population in terms of urban/rural location and deprivation, we acknowledge a number of potential sources of bias. These include, that only six practices were involved and a marginally higher proportion of patients aged over 69 years compared to the national population. In addition, it is unlikely that all surgery consultations were included as more than one patient may have been seen during a single consultation and urgent consultations may not have been documented. We extrapolated the telephone and out of hours consultation rate (calculated directly from practice management software or returns from the deputising service) from one practice to all six practices. It should be noted that the calculated ‘out of hours’ consultation rate for this practice was 0.2 per GMS patient; lower than what one would expect from national data of 804,670 out of hours GMS payments in 2011 for a total population of 1,819,720 GMS patients.
It is generally accepted that general practice and primary care are key to the reconfiguration of health services in Ireland in order to provide a more responsive, cost effective health service. Accurate data on workload, morbidity and health service utilisation is necessary to reliably inform these changes. Current official data, which is produced by survey and does not consider data contained in general practice based information systems, appears to greatly under-reflect workload in general practice, both current and future. Significant changes in national health policy should only be made if the data supporting the transformation is both reliable and convincing. Utilising current official data to plan future work-load will lead to very unpredictable results.
Acknowledgements
Colleagues at the six participating practices who collected data for this study and staff at Walkinstown Primary Care Centre for their support and help with the project. Data analysis and manuscript drafting was assisted by the Graduate Entry Medical School at University of Limerick.
Correspondence: W Behan
Walkinstown Primary Care Centre, 115 Cromwellsfort Road, Dublin 12
Email: [email protected]
References
1. 43.3% Population possess medical cards. Dáil Éireann Debate. Discretionary Medical Cards: Motion [Private Members] (Continued)Tuesday, 8 October 2013
http://oireachtasdebates.oireachtas.ie/debates%20authoring/debateswebpack.nsf/takes/dail2013100800047?opendocument (Accessed 03 November 2013.).
2. Statistical Analysis of Claims and Payments http://www.hse.ie/eng/staff/PCRS/PCRS_Publications/pcrsclaimsandpayments2011.pdf (Accessed 22 October 2013.). Dublin: Health Service Executive. Primary Care Reimbursement Service. 2011.
3. Doctors and Dentists Survey http://corporate.nca.ie/eng/Research_Zone/price-surveys/NCA-Doctors-Dentists-Report-may2010.doc (Accessed 11 November 2013). Dublin: National Consumer Agency, 2010.
4. Health Status and Health Service Utilisation, Quarterly National Household Survey http://cso.ie/en/releasesandpublications/health/archive/ (Accessed 22 October 2013.). Dublin: Central Statistics Office2007.
5. Health Status and Health Service Utilisation, Quarterly National Household Survey http://cso.ie/en/releasesandpublications/health/ (Accessed 22 October 2013.). Dublin: Central Statistics Office, 2010.
6. European health interview survey (EHIS). Reference Metadata in Euro SDMX Metadata Structure (ESMS). http://epp.eurostat.ec.europa.eu/cache/ITY_SDDS/en/hlth_ehis_esms.htm (Accessed 22 October 2013.): Eurostat, the statistical office of the European Union.2008.
7. Health, Quarterly National Household Survey. http://cso.ie/en/media/csoie/releasespublications/documents/labourmarket/2001/qnhs_healthqtr32001.pdf (Accessed 22 October 2013.). Dublin: Central Statistics Office2001.
8. Statistical Analysis of Claims and Payments 2010. http://www.hse.ie/eng/Staff/PCRS/PCRS_Publications/20108_Report.pdf (Accessed 22 October 2013.). Dublin: Health Service Executive. Primary Care Reimbursement Service. .
9. Statistical Analysis of Claims and Payments 2009. http://www.hse.ie/eng/Staff/PCRS/PCRS_Publications/2009_Report.pdf (Accessed 22 October 2013.). Dublin: Health Service Executive. Primary Care Reimbursement Service. .
10. Statistical Analysis of Claims and Payments 2008. http://www.hse.ie/eng/Staff/PCRS/PCRS_Publications/2008_Report.pdf (Accessed 22 October 2013.). Dublin: Health Service Executive. Primary Care Reimbursement Service. .
11. Statistical Analysis of Claims and Payments 2007. http://www.hse.ie/eng/Staff/PCRS/PCRS_Publications/2007_Report.pdf (Accessed 22 October 2013.). Dublin: Health Service Executive. Primary Care Reimbursement Service. .
12. Hippisley-Cox J, Vinogradova Y. QResearch and The Health and Social Care Information Centre. Final Report to the NHS Information Centre and Department of Health. Trends in Consultation Rates in General Practice 1995/1996 to 2008/2009: Analysis of the QResearch database
http://www.hscic.gov.uk/searchcatalogue?productid=729&topics=1%2fPrimary+care+services%2fGeneral+practice&sort=Most+recent&size=100&page=1#top (Accessed 22 October 2013.). 2009.
13. Power C, O'Connor R, Dunne S, Finucane P, Cullen W, Dunne C. An evidence-based assessment of primary care needs in an economically deprived urban community. Ir J Med Sci. 2013 Sep;182:457-61.
14. Glynn LG, Valderas JM, Healy P, Burke E, Newell J, Gillespie P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Family practice. 2011 Oct;28:516-23.
15. O'Dowd T, O'Kelly M, O'Kelly F. Structure of General Practice in Ireland: 1982-2005. Dublin: ICGP / TCD2005.
16. Programme for Government. Dublin: Oireachtas2011.
17. Fitzpatrick F, Harrington P, Mahony D. The "silver-haired" general medical services patient. Clinical activity of the non-means tested over-70's during their first six months. Ir Med J. 2004 Apr;97:111-4.
18. Nolan A. Evaluating the impact of eligibility for free care on the use of general practitioner (GP) services: a difference-in-difference matching approach. Social Science and Medicine. 2008;67 (1164-1172 ).
19. Brick A, Nolan A, O’Reilly J, Smith S. Resource Allocation, Financing and Sustainability in Health Care. Evidence for the Expert Group on Resource Allocation and Financing in the Health Sector http://www.esri.ie/UserFiles/publications/BKMNEXT167V2.pdf (Accessed 22 October 2013.). Dublin-: Economic and Social Research Institute2010.
20. CSO statistical release, 29 August 2013, Population and Migration Estimates. Apr-13. Table 5 Estimated Population classified by Sex and Age Group, 2008 - 2013
