Introduction
Healthcare staff who smoke are less likely to advise patients to quit.1 There is limited national information on the number of healthcare staff who smoke,2-4 or of their awareness of cessation supports. This national study was carried out to address these gaps.
Methods
1,064 HSE staff, stratified by staff category, were randomly selected to receive a pre-piloted postal questionnaire on their smoking status and their knowledge of cessation supports in April 2012. To maximise the response rate, cover letters were personalised, reply-paid envelopes were included and two reminders were sent. Data were analysed in SPSS® version 20.
Results
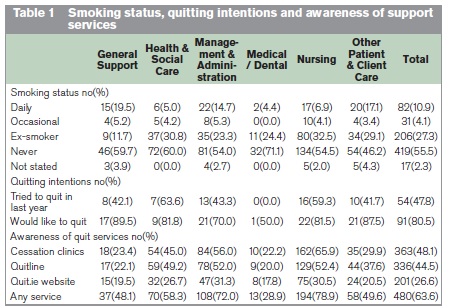
From the 1,064 questionnaires, 755 (71.0%) valid responses were received. The overall smoking prevalence was 15.0% (10.9% daily, 4.1% occasional), range: 4.4% (Medical/Dental) to 24.7% (General Support staff), Table 1. Front-line healthcare staff (Health & Social Care, Medical/Dental and Nursing) were 2.5 times less likely to smoke (adjusted odds ratio 0.38, p<0.001) than other staff categories, while General Support staff were almost twice as likely to be current smokers (adjusted OR 1.93, p=0.026). Of the 113 smokers, 54 (47.8%) had tried to quit in the previous year, and 91 (80.5%) expressed a desire to quit. 63.6% of staff were aware of quit services, ranging from 28.9% of Medical/Dental to 78.9% of Nursing staff. Medical/Dental staff (adjusted OR 0.25, p<0.001) were less likely to be aware of quit services, as were General Support staff (adjusted OR 0.43, p=0.002). Only 20.0% of Medical/Dental and 22.1% of General Support staff were aware of the Quitline.
Discussion
With a smoking prevalence of 15.0%, HSE staff are less likely to smoke than the population aged 18-65 years (24.2%),5 but General Support staff smoke just as much as the working population and do not seem to enjoy any “protective benefit” against smoking from working in the health sector. Whilst the smoking prevalence estimate of 4.4% among Medical/Dental staff is lower than the 21.7% observed among non-consultant hospital doctors in 2006,3 it is close to the estimate of 5.0% among all medical staff in the same year.2 It is reassuring that nurses and Health & Social Care staff (which includes psychologists, dieticians and social workers) exhibit a relatively low smoking prevalence, as they may have opportunities to support smokers who wish to quit. This study’s estimated smoking prevalence of 11.0% among Nursing staff is less than previous estimates of 21%6 and 22.5%.2 This difference may be explained by successful cessation; this audit found that 32.5% of Nursing staff were ex-smokers. Our estimated smoking prevalence of 5.0% among Health & Social Care staff approximates Fitzpatrick’s estimate of 2.5% among Allied Health Professionals.2
The smoking status of healthcare workers is important because they are seen as a model for patients and clients of the health services.2 In addition, because smoking is associated with impaired perceptions of the risks of smoking, negative attitudes to cessation, and a diminished desire for training in smoking cessation,1,6,7 it is important that healthcare workers are encouraged and facilitated to quit. There is a strong trend for healthcare workers to quit: 27.3% are now ex-smokers. So, for every current smoker, almost two have quit. It is encouraging that four-fifths of smokers wish to quit, and that half of them had attempted to quit in the last 12 months. It is important that healthcare staff are aware of the cessation support services available for themselves and the smoking population. Unfortunately, less than two-thirds are aware of any cessation service. In particular, only 28.9% of Medical/Dental staff were aware of quit services. The low level of awareness among Medical/Dental staff suggests that they are not fully equipped to direct their smoking patients or clients to relevant services.
It is important that the HSE provides incentives and supports to motivate and encourage all smoking staff to quit. In particular, targeted interventions are required to support General Support and Other Patient & Client Care staff in smoking cessation. In addition, the HSE must ensure that all its staff are aware of the supports that are available to patients who wish to quit and that they have the relevant skills training to help their patients quit. Finally, the finding that less than 5% of doctors/dentists smoke underscores the point that a tobacco-free Ireland (population smoking prevalence <5%) could be achieved by 2025.
Correspondence: CO ÓhAiseadha
c/o Department of Public Health, Dr Steevens' Hospital, St John's Rd West, Dublin 8
Email: [email protected]
Acknowledgements
All the members of staff of the HSE who gave of their time to take part in this audit; staff at the Human Resources Department, the National Tobacco Control Office and the Department of Public Health, Navan, for their assistance in conducting this work.
References
1. Pipe A, Sorensen M, Reid R. Physician smoking status, attitudes toward smoking, and cessation advice to patients: an international survey. Patient Education and Counseling. 2009;74:118-23.
2. Fitzpatrick P, Gilroy I, Doherty K, Corradino D, Daly L, Clarke A, Kelleher CC. Implementation of a campus-wide Irish hospital smoking ban in 2009: prevalence and attitudinal trends among staff and patients in lead up. Health Promotion International. 2009;24:211-22.
3. Naji N, McLoughlin H, Connell F, Clancy L. Smoking profile of non-consultant hospital doctors. Irish Journal of Medical Science. 2006;175:29-31.
4. O’Cathail M, O’Callaghan M. A profile of hospital consultants: The health practices of a cohort of medical professionals. Irish Medical Journal. 2013;106.
5. National Tobacco Control Office. Ireland: Current trends in cigarette smoking. Naas, Ireland, 2013. Available from: http://www.ntco.ie/research.asp
6. O'Donovan G. Smoking prevalence among qualified nurses in the Republic of Ireland and their role in smoking cessation. International Nursing Review. 2009;56:230-6.
7. Slater P, McElwee G, Fleming P, McKenna H. Nurses' smoking behaviour related to cessation practice. Nursing Times. 2006 May 9-15;102:32-7.