Abstract
The objective of this project was to analyse the current access to in-patient stroke services and MDT rehabilitation in an acute stroke centre and to compare these services to the recommended “National Clinical Guidelines and Recommendations for the Care of People with Stroke and TIA” (IHF 2010). A retrospective chart review was carried out, recording activity statistics of all patients admitted with acute stroke over a three-month period. 73 patients (male=40, 54.8%) were included. Patients were discharged from the stroke service after a mean stay of 20.2 days (SD.= 19.3). 76.7% (N=56) of patients were admitted to the acute stroke unit (ASU). The mean length of time from admission to first assessment 3.4 days (SD.=2.68), with an average of 138 minutes of treatment received per day across all disciplines. This is compared to the IHF’s recommendation of patients being assessed within 24-48 hours of admission and receiving 180 minutes of treatment across all disciplines. As demands for stroke MDT services increase, it is important to recognise the benefits of increasing staff and resources to maintain and continue to improve standards of care.
Introduction
Stroke is the third most common cause of death and the most common cause of acquired major physical disability in Ireland1. There is a very high incidence of stroke, with nearly 11,000 new cases in Ireland every year2. In 2007, the Cost of Stroke in Ireland (COSI) report showed that less than €7 million per year is being spent on rehabilitation of survivors of stroke, an average spend of just over €200 per person3. It was proposed that improvements in acute stroke services could save 750 people per annum from lifelong dependency or death, and lead to a saving of €13 million per annum3. The Irish Heart Foundation Guidelines for Stroke Care suggested that, after having a stroke, patients should be cared for in a dedicated stroke unit4.
An Acute Stroke Unit (ASU) is a specialised unit dedicated to the treatment of stroke5. Previous studies have shown that patient care is greatly enhanced by treatment in a stroke unit regardless of a patient’s age, gender or the severity of their stroke6. The first Irish National Audit of Stroke Care (INASC) in 2006-2007 found that only one hospital, of 37 (3%) in Ireland had a fully operational stroke unit7.There are currently 28 acute hospitals with operational stroke units; however some of these may be operating with incomplete multidisciplinary team (MDT) input8. Stroke has widespread effects on physical function but also on cognitive and emotional function and ability to communicate. An MDT approach is needed to assess and meet these challenges. The results of INASC highlighted limited access to the MDT7. The objectives of this project were to analyse the current access to in-patient stroke services and MDT rehabilitation in an acute stroke centre and compare these services to the current best practice guidelines, as set out by the Irish Heart Foundation (IHF) (2010)4.
Methods
A retrospective analysis was carried out of the acute stroke service at Beaumont Hospital, Dublin. Patients admitted to Beaumont Hospital with acute stroke (infarction or haemorrhage), over a three-month period (March-May 2012) were included in the study. Therapy activity statistics were kept for all patients admitted, including time spent with each patient and interventions implemented by the medical and MDT. Demographic information, stroke type, length of stay in the ASU and the hospital were recorded for these patients using a standardised proforma derived from the IHF and local stroke care guidelines. Information was retrieved from hospital charts, hospital computer statistic programmes, the Patient Information Profile Explorer (PIPE) and through discussion with the MDT. Results were analysed using Microsoft Excel. The study was approved by the Beaumont hospital Clinical Governance and Audit Office.
Results
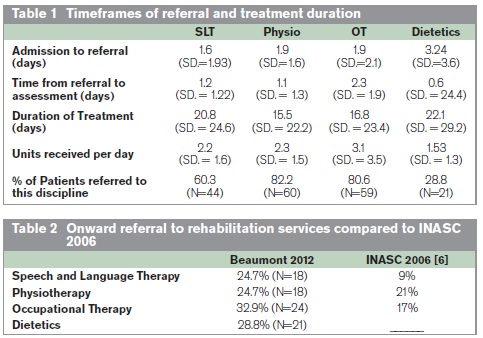
73 patients (male=40, 54.8%) were included in this study. Three quarters (76.7%, N=56) of patients were admitted to the acute stroke unit (ASU). Patients spent on average over 2-weeks in the ASU (14.6 days, SD.=15.1). The mean time from admission to MDT referral was less than 2 days and the mean time from referral to assessment approximately 1 day. The length of treatment varied across disciplines, but was on average 1-2 weeks in duration. Table 1 outlines the average times for referral, assessment and treatment for each discipline.
Speech and Language Therapy
60.3% (N=44) of patients were referred for speech and language therapy (SLT) and 41.5 % of those (N=17) were reviewed for swallowing in the first 24 hours using the Beaumont Hospital Swallowing Screening Tool (BHSST). 22% (N=9) of patients referred did not receive the BHSST test as they were not admitted to the ASU, the only location in the hospital where this test was performed at the time of this study. 24.4 %(N=10) had a formal swallowing review by SLT within 24 hours of admission with a further 24.4% (N=10) reviewed within 24 hours of referral being received. An additional 7.3% (N=3) were reviewed within 48 hours of referral being received. Similar results were found for assessment of communication problems by the SLT. Treatment concentrated on swallow deficits the first 2 weeks after stroke while patients also received treatment for communication deficits.
Physiotherapy
82.2%(N=60) were referred for physiotherapy. Of these patients 42.9% (N=24) received an initial assessment within 24 hours of admission and a further 33.9% (N=9) were seen within 24 hours of referral. Reasons for delays in assessment included patients being unwell (5.4%, N=3) and referrals sent over the weekend (5.4%, N=3). 55.4% (N=31) of patients received a full physiotherapy assessment within 5 days of admission, with a further 5.4% (N=3) seen within 5 days of receipt of referral. Delays were mainly due to patients being unwell (8.9%, N=5). Physiotherapy treatment focussed on transfer practice, balance and mobility over the first 2 weeks of therapy.
Occupational Therapy
80.8% (N=59) were referred to occupational therapy (OT) and 58.9% of these of patients had an initial assessment within 48 hours of admission. A further 21.7% were seen within 48 hours of the referral being received. Reasons for not being seen on time included patients being too unwell (5.4%, N=3) and referrals being sent over the weekend (12.5%, N=7). Occupational therapy included assessing Personal Activities of Daily Living (PADLs), upper limb rehabilitation, vision and perception, cognition and functional mobility, especially over the first 2 weeks of treatment. OT was also involved in assessing Domestic Activities of Daily Living (DADLs) and discharge planning.
Dietetics and Nutrition
28.8% (N=21) of patients were referred to Dietetics and Nutrition. 57%(N=12) of those patients were referred to the Dietician within 48 hours of admission, and 42.9% (N=9) were weighed. All were receiving nutrition within 72 hours of admission and the following interventions were used: Artificial Nutritional Support (60%, N=12), modified consistency (10%, N=2), high protein high calorie (10%, N=2), secondary prevention (20%, N=4). Secondary prevention included diabetic diets and low cholesterol diets.
Onward referral at discharge
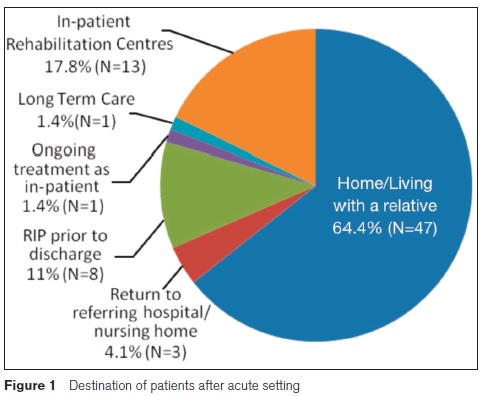
54.7% (N=35) of discharged patients were referred for further rehabilitation by the MDT, SLT 24.7% (N=18), physiotherapy 24.7% (N=18), Dietetic 28.8%(N=21) and OT 32.9% (N=24). Patients were referred to a variety of services, including community care, in-patient rehabilitation and out-patient rehabilitation services. Nearly 17% (N=11) of patients that were discharged to the hospital’s off site rehabilitation unit at St Joseph’s Rehabilitation Unit Raheny. On discharge, nearly two-thirds (64.4%, N=47) of patients went home or to live with their families, 17.8% (n=13) went to in-patient rehabilitation, and 4.1%(N=3) returned to their referring hospital/nursing home. Just 1.4% (N=3) were still in-patients at the time of this study (Figure 1).
Discussion
Beaumont hospital has an ASU with a dedicated team, however only 76.7% (N=56) of stroke patients admitted to the hospital were admitted to the ASU. The IHF National Stroke Care Guidelines suggest that all stroke patients should be treated in an Acute Stroke Unit4,6. Beaumont hospital recommends that patients should spend the first 72 hours of their acute treatment of stroke in the ASU. After this, the patients, if well enough, should be moved to another ward for ongoing rehabilitation. During this study period patients spent an average of 14.6 (SD= 15.1) days in the ASU. If this length of stay was shorter than the percentage of patients that were not admitted to the ASU may be reduced. Patient care is greatly enhanced by treatment in a stroke unit6, thus it would be of benefit to the patient to spend their initial treatment time in the ASU. There are many reasons that could affect this length of stay, including bed availability on other wards, the extent of the illness of the individual patients and the needs of patients to continue receiving specialised care, which may only to be available within the ASU.
Patients who were not admitted to the ASU did not receive an initial swallow screening test. At the time of the study, only the nurses who worked in the ASU were trained to do this test. It may be of benefit to teach staff on different wards managing stroke patients how to do this test following appropriate training. The typical patient who was treated by all four disciplines received approximately 138 minutes of direct care. The IHF guidelines suggest that patients are offered a minimum of 45 minutes of each active therapy for a minimum of five days a week4. This means each patient who is being seen by all four disciplines should receive 180 minutes per day. Currently many patients are not receiving the recommended amount of treatment. This study showed higher levels of onward referral to rehabilitation than INASC, where there was limited evidence of onward referral to rehabilitation services7. It has been reported that intensive rehabilitation up to 6 months may lead to improvements in mobility and activities of daily living9 highlighting the need for timely onward referral for patients to improve outcome.
The length of time from admission until referral to MDT, and referral to first assessment was longer than the recommended 24 hours in the IHF guidelines. There was generally a two-day delay for patients to be referred to the appropriate services and the patients are seen within 24-48 hours of referral being received. Reasons for non-compliance with the guidelines varied, including referrals being sent at weekends and patients being too unwell to engage in rehabilitation. Furthermore there appeared to be a longer period of time until referral to Dietetics, 3.24 (SD. 3.6) days compared with less than 2 days for other disciplines. It is unclear as to why this was the case. All disciplines responded to referrals in accordance with local guidelines with dietetics, physiotherapy and SLT responding within 1 day and OT responding within 2 days for most patients. No discipline provided an average of 45 minutes of treatment daily per patient with the exception of OT. The provision of longer daily treatment within the current health setting, although in accordance with the guidelines, may be partially the reason for an extended response time to referral. The longest duration of treatment was for patients referred to dietetics and SLT, which may be indicative of patients continuing to display swallowing difficulties and requiring ongoing nutritional support. This is one example of the high interdependence between the MDT members. While it is important to refer patients promptly, it is also important to refer patients appropriately. At the weekly meetings, the MDT discuss all patients referred to the each discipline. It was decided at these meetings that some of these patients did not require therapy from these disciplines: SLT (6.8%), Physiotherapy (6.7%), Occupational therapy (5.1%) and Dietetics and Nutrition (4.8%).
As demands for stroke MDT services increase, it is important to recognise the benefits of increasing staff and resources to maintain and continue to improve standards of care. However, it must be acknowledged that in the current economic climate this will be challenging and the existing resources may be stretched. Training of more staff to conduct an initial screening for swallow disorders has been recognised as an area of potential improvement in this hospital. This should increase the number of patients that receive this screening off the ASU. A more precise estimate of interval in hours rather than days would be preferable in this study. This would provide a more accurate picture of the overall system and highlight the areas of delay of treatment.
Correspondence: E O'Sullivan
Derrymaclavode, Clonkeen, Killarney, Co Kerry
Email: [email protected]
Acknowledgements
This research was funded by the RCSI Summer Student Research Programme Alumni (2012), ‘Irish Medicines Board (IMB) Research Award’.
References
1. Irish Heart Foundation, “Irish Heart Foundation National Audit of Stroke Care” 2008.
2. Irish Heart foundation. http://www.irishheart.ie/ (accessed 10 June 2013)
3. Smith S, Horgan F, Sexton E, Cowman S, Hickey A, Kelly P, McGee H, Murphy S, O'Neill D, Royston M, Shelley E, Wiley MM. (2010) COSI (Cost of Stroke in Ireland: Estimating the Annual Economic Cost of Stroke and TIA in Ireland), Dublin: The Irish Heart Foundation. http://www.esri.ie/publications/latest_publications/view/index.xml?id=3090
4. Irish Heart Foundation: Council for Stroke, “National Clinical Guidelines and Recommendations for the Care of People with Stroke and Transient Ischaemic Attack”, March 2010.
5. Steiner T, Juvela S, Unterberg A, Jung C, Forsting M, Rinkel G. European Stroke Organisation Guidelines for the Management of Intracranial Aneurysms and Subarachnoid Haemorrhage.Cerebrovasc Dis 2013; 35: 93-112.
6. Jørgensen HS, Kammersgaard LP, Houth J, Nakayama H, Raaschou HO, Larsen K, Hu¨bbe P, Olsen TS. “Who Benefits From Treatment and Rehabilitation in a Stroke Unit? - A Community-Based Study”. Stroke 2000;31;434-439.
7. INASC (Irish National Audit of Stroke Care). Specific Reports, Hospital Surveys: Organisational Audit; Hospital Chart Audit Report. Community Audit: National Survey of General Practitioners: National Survey of Allied Health Professionals and Public Health Nurses; Survey of Patients and Carers; National Nursing Home Survey. 2006; www.irishheart.ie.
8. Gary Culliton (January 2012) 'Five new stroke units planned', Irish Medical Times, [Online]. Available at: http://www.imt.ie/news/latest-news/2012/01/five-new-stroke-units-planned.html (Accessed: 11/10/2012).
9. Kwakkel G, van PR, Wagenaar RC, Wood DS, Richards C, Ashburn A, Miller K, Lincoln N, Partridge C, Wellwood I, Langhorne P. Effects of augmented exercise therapy time after stroke: a meta-analysis. Stroke. 2004;35:2529 –2539.
