Introduction
Ireland still continues to rank amongst the highest consumers of alcohol in Europe, with the average Irish adult drinking 11.3 litres of pure alcohol in 20092. As part of the Programme for Government 2007-20123, the Government agreed to: “Provide early intervention programmes in all social, health and justice services to ensure early detection and appropriate responses to high risk drinking”. The purpose of early intervention programmes is to detect high risk and harmful drinking in individuals, before or shortly after the early signs of alcohol related problems. This action led to the decision by the Health Service Executive former Population Health Directorate to designate “Towards a Framework for Implementing Evidence based Alcohol Interventions” as one of its transformation projects.
There is clear and conclusive evidence that the problems from consumption levels are reflected in both admissions to general hospitals4-7 and attendances at emergency departments7-9. Hope et al9 proposed that between 20% and 50% of all presentations to emergency departments in Ireland are alcohol related, with the figure rising to over 80% at peak weekend periods. The initial focus of the project was to test feasibility of screening and brief intervention (SBI) within emergency departments. In February, 2008 a mapping exercise was undertaken with all acute hospitals nationally. The results of this exercise showed the level of response to alcohol related attendances and helped to identify acute hospitals where significant interventions were already in place. A national meeting with persons interested in alcohol in the acute hospital setting took place in June, 2008. The mapping document and national meeting identified seven hospitals where the feasibility test could be carried out. Multi-disciplinary meetings were held with staff in seven hospitals and four of the seven hospitals were able to test feasibility of SBI in the emergency department.
Methods
Staff were briefed on the project in four hospitals and agreed that over the period December 2009 to February 2010, they would administer the screening tool and deliver appropriate interventions. The M-SASQ (modified-single alcohol screening question) screening tool was selected for use within the hospital emergency departments. This is a single question screening tool, which uses question 3 from the Alcohol Use Disorders Identification Test (AUDIT). The AUDIT10 screening tool is considered the gold standard of screening tools internationally. However, it contains ten questions and is considered time consuming to administer. The SIPS11 (Screening and Intervention Programme for Sensible Drinking) programme in the UK developed the M-SASQ screening tool from the original Single Alcohol Screening Question (SASQ)12,13. The tool was modified and adapted to Ireland’s standard drinks (1 drink= 10g of ethanol). Testing in the SIPS pilot study11 showed M-SASQ has a higher sensitivity and specificity than the original SASQ (Sensitivity 91.8; Specificity 70.8; AUC 0.929) when compared to the gold standard AUDIT during a pilot study within this wider SIPS programme. Nurses in hospitals A, B and C administered the M-SASQ screening tool in the emergency department, while Hospital D administered the tool in the Clinical Decisions Unit. Hospitals A, B and C administered the screening sheet through triage and also by requesting patients to self-complete the form for discussion with a doctor or a nurse.
Results
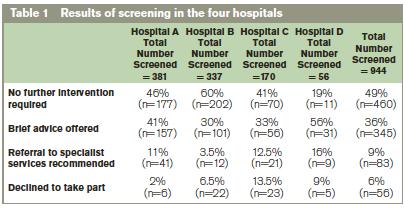
A total of 944 patients across four learning sites were screened for hazardous and harmful alcohol use (Table 1).The results showed that there was good co-operation from the public with 94% of people agreeing to be screened. The screening tool detected that 49% of people needed no intervention, 36% needed brief advice and 9% required referral to specialist services. This shows the value of the screening but also helps to reassure staff that people were happy to take part.
Discussion
The response towards the project was positive in all hospitals and there was an acceptance among all staff that alcohol is a problem for emergency departments. Staff felt that alcohol was by far the main drug problem encountered in their work and in some areas staff cited an increase in poly drug use, particularly cocaine and alcohol use. All agreed that there was value in screening and delivering brief interventions particularly as some staff felt that alcohol was becoming an increasing problem in emergency departments. While the aim of the project was to screen everyone attending the emergency department, it was acknowledged at the outset that there are certain circumstances where this is not feasible for staff. Examples given were; patients drunk on arrival in the emergency department, seriously ill patients, refusal to co-operate, confused or agitated patients, nursing home/residential care unit patients and patients detained under the Mental Health Act, 200114. At all times screening was left to the discretion of staff in the individual hospitals and patients could also decline to be screened. Staff concerns about patient refusal proved to be unfounded as only 6% declined to be screened. This figure is further supported by a survey15 which found that there is near complete support (95% or over) for healthcare professionals asking about alcohol consumption where there is a link to the condition or treatment. While there is less support in the context of routine history taking, support remains strong at 89 %.
As screening for alcohol use was likely to identify some patients requiring referrals to specialist services, local alcohol and addiction services were informed of the project prior to the commencement of the feasibility test. The number of patients requiring referral was lower than anticipated by staff at 9%. A localised media campaign accompanied the rollout of the project in the participating hospitals and included press releases, interviews with local media and posters displayed in waiting rooms. The aim of the media campaign was to inform the general public that this test was taking place in selected hospitals and if they attended the emergency department in their local area they would be asked about their alcohol use.
Staff displayed a positive attitude and willingness to participate in the test and were committed despite the barriers they encountered within their work environment. Emergency departments are by their very nature busy environments and at the time of the SBI rollout there were additional strains placed on resources with the H1N1 virus and severe winter weather resulting in an increase in emergency department attendances. The identification of a local “champion” at each site was vital to the roll out of SBI within the emergency department. In some cases the alcohol/substance misuse liaison nurses and liaison psychiatrists fulfilled this role, providing invaluable information on existing alcohol interventions within the hospital and acting as a liaison between the project team and relevant staff within the hospital. In other cases the “champion” role was fulfilled through a combination of support from the local addiction services, psychiatric liaison service and the health promoting hospital co-coordinator or emergency department nurse manager. This led to a co-coordinated effort within the emergency department. The value of the work provided by alcohol/substance misuse liaison nurses and other services cannot be underestimated.
The feasibility test also highlighted the challenges of implementing SBI in the emergency department. Prior to the feasibility test seven hospitals were identified as appropriate sites. However, only four committed to the test. Of the three hospitals that declined to take part, one hospital cited understaffing as the reason, another was experiencing a period of staff rotation and the final hospital questioned the ethics of the project. Ethical approval had not been sought for the project, as it was not research based. As a result of the ethical issue being raised the authors sent a copy of the project protocol to the Chairperson of the Public Health Medicine/Occupational Medicine Research Ethics Committee of the Royal College of Physicians of Ireland. The Chairperson replied that in his view the project did not require ethical approval as it was a service and not a research issue. However, as the issue had been raised each of the four participating hospitals' ethics committees was asked to consider the project and ethical approval was granted.
Following the feasibility test, staff expressed considerable concern regarding time constraints for delivering SBI. Staff felt that alcohol is a sensitive issue for a lot of patients and the emergency department environment is not always conducive to delivering a brief intervention. The need for privacy was referred to, along with delivering a worthwhile intervention. There was a perceived benefit from having a dedicated member of staff to provide information and support and who has allocated time to provide an intervention. The existence of an alcohol/substance misuse liaison nurse meant that staff had already been exposed to alcohol awareness training and in some cases brief intervention training. In the absence of an alcohol liaison nurse, other services such as local drug and alcohol services or health promotion hospital coordinators provided training support to hospitals. Where alcohol awareness training had been provided, staff reported that they were more comfortable asking about alcohol use. Training is essential for staff to feel competent and confident in delivering SBI. A training programme was offered to all participating hospitals and the SAOR16 model of training for SBI for alcohol in the emergency department & acute care settings was selected. The SAOR acronym (Support, Ask and Assess, Offer assistance and Refer) offers a four step model for the delivery of SBI which guides practitioners in the emergency department and other acute hospital settings through brief intervention in a flexible and adaptable manner. During discussions with staff at hospital visits, several barriers to training were highlighted, in particular the release of staff to attend training and the length of training courses. Flexible options for training delivery are now required; in practice onsite and e-learning programmes are the only practical options for emergency department staff. The SAOR model of training provided an appropriate training tool for introducing SBI to the emergency department and verbal feedback from the hospitals was positive.
The single item M-SASQ screening tool proved popular with staff and as envisaged, staff reported that the screening tool itself was the best option for a busy emergency department. Administering a longer screening tool was not deemed practical in an emergency department but staff felt that this might be possible in other hospital wards or in a self-administered computerised test based in the emergency department. Overall, staff reported that the M-SASQ screening tool was user friendly and quick and easy to administer. They also felt that a single item question could be more easily included in standard patient documentation, both paper and electronic. The inclusion of screening questions in emergency department and patient documentation would help with the recording of data and follow up with the patient. Proposals have been put forward in some of the hospitals to have alcohol documentation included in the standard patient documentation. This exercise has demonstrated that there is much benefit in systematic screening for alcohol in Emergency Departments as our drinking patterns are such that much morbidity can be prevented. Ideally, the screening should become part of the normal clinical assessment.
Correspondence: R Armstrong
HSE, Oak House, Millennium Park, Naas, Co Kildare
Email: [email protected]
Acknowledgements
All the staff in the four hospitals who assisted us during the feasibility test.
References
1. World Health Organization. Global status report on alcohol and health. Geneva: WHO; 2011.
2. OECD (2010) OECD Health Data 2010- Frequently Requested Data accessed June 2011 at http://www.oecd.org/document/16/0,3746,en_2649_34631_2085200_1_1_1_1,00.html
3. Working Party of the Royal College of Physicians. Alcohol - can the NHS Afford it? Recommendations for a Coherent Alcohol Strategy for Hospitals. London: Royal College of Physicians. 2001.
4. Hearne R, Connolly A, Sheehan J.A & E nurses and alcohol related attendances. Nurs Times. 2002; l: 59 – 62.
5. Molyneux GJ, Cryan E, Dooley E. The point prevalence of alcohol use disorders and binge drinking in an Irish general hospital. Irish J Psychol Med. 2006; 23 (1): 17-20.
6. Hope A. Alcohol-related Harm in Ireland. Dublin: Health Service Executive. 2008.
7. Charalambous M. Alcohol and the accident and emergency department: a current review Alcohol Alcsm.2002; 37: 307 – 312.
8. Hope A, Gill A, Costello G, Sheehan J, Brazil E, Reid V. Alcohol and Injuries in the Accident and Emergency Department: A National Perspective. Dublin: Department of Health and Children, 2005.
9. Department of the Taoiseach. Programme for Government 2007-2012. Dublin: Stationary Office, 2007.
10. World Health Organization . The Alcohol Use Disorders Identification Test-Guidelines for Use in Primary Care. Geneva: WHO; 2001.
11. Screening and Intervention Programme for Sensible Drinking (SIPS) [Internet] UK: National Addiction Centre; 1999-2008 [cited 2009 July 4] Available from http://www.sips.iop.kcl.ac.uk/msasq.php
12. Williams RH, Vinson DC (2001) Validation of a single question screen for problem drinking. J Fam Practice. 2001; 50: 307–312.
13. Canagasaby A, Vinson D. Screening for hazardous or harmful drinking using one or two quantity-frequency questions. Alcohol Alcsm. 2005; 40: 208-213.
14. Mental Health Act, Ireland [statute on the Internet].c2001 [cited 2011 July 8]. Available from http://www.irishstatutebook.ie/2001/en/act/pub/0025/index.html
15. Health Research Board. Alcohol: Public Knowledge, Attitudes and Behaviour. Dublin: Health Research Board, 2012.
16. O’Shea J, Goff P. SAOR Model of Screening and Brief Intervention. Dublin: Health Service Executive. 2009.
