Discussion
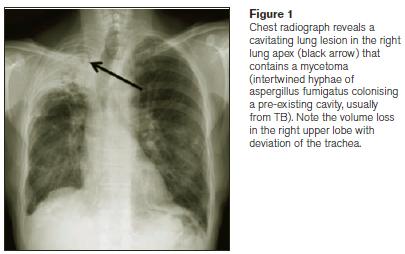
Cavitation is a common complication of tuberculosis (TB) infection of the lungs. It is usually located in the upper lobes and superior segments of the lower lobes, often in the presence of other imaging findings of granulomatous infection. In the presence of a chronic lung cavity, secondary infection with aspergillus (usually a. fumigatus) can occur. It typically occurs in a cavity caused by prior TB but may however occur in association with lung bullae, sarcoidosis or other cavitatory lung disease. Pulmonary manifestations of aspergillus infection include aspergilloma, semi-invasive aspergillosis, angio-invasive aspergillosis and invasive tracheobronchial aspergillosis1. Most mycetomas (or fungal balls) are aspergillomas, and in fact these terms are often used interchangeably. They generally develop in a pre-existing lung cavity in immunocompetent individuals following inhalation of airborne spores. The clinical disease spectrum ranges from the completely asymptomatic patient with aspergilloma, as in this case, to presentation with life-threatening haemoptysis2.
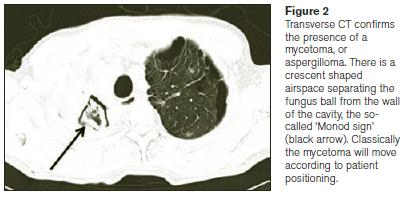
Diagnosis can be made with sputum culture and bronchoalveolar lavage, however occasionally requires transthoracic or open lung biopsy. A serum aspergillus precipitin test and elevated serum galactomannan (an aspergillus cell wall component) levels are also helpful in the diagnosis of aspergillosis3. Imaging findings include a fungus ball or sponge-like mass within an existing cavity (representing hyphae, mucous and fibrin), often with a surrounding crescent of air, the so-called Monod sign. It may be mobile within the cavity and change position depending on patient positioning, or may fill the entire cavity. In asymptomatic patients no treatment is warranted and patients should be managed expectantly. In symptomatic patients anti-fungal therapy with voriconazole has been attempted with variable reported degrees of success4. Bronchial artery embolization may be employed to control haemoptysis. In severe cases, surgical resection may be the only viable option, but this is associated with considerable mortality, especially if there is significant co-existing pulmonary disease5.
Semi-invasive pulmonary aspergillosis, also known as chronic necrotizing pulmonary aspergillosis, is a sub-acute disease seen in immunosuppressed patients, for example patients on steroids, with diabetes, alcoholism and occasionally in the setting of sarcoidosis. CT findings include nodules, masses and consolidation. Angio-invasive pulmonary aspergillosis usually occurs in febrile, neutropenic patients and has characteristic CT findings of pulmonary nodules with surrounding ground-glass change, the so-called halo sign representing surrounding pulmonary haemorrhage. When the infection starts to clear and a granulomatous response ensues, air is seen to surround a part of the nodule giving the so-called ‘air-crescent sign’, a sign that indicates effective treatment and a favourable outcome6. This is not to be confused with Monod’s sign of a crescentic slip of air around a mycetoma, as mentioned earlier. Other fungal infections to consider in the immunosuppressed patient are invasive candidiasis and mucormycosis.
Allergic bronchopulmonary aspergillosis (ABPA) is a separate disease entity that is essentially an abnormal immune response to aspergillus spores, almost always in patients with underlying lung disease, such as asthma or bronchiectasis. The cause of the mycetoma in our patient was felt to be secondary to prior TB infection. He did very well following treatment with anti-fungal agents and remains asymptomatic.
Correspondence: S Gaine
Department of Respiratory Medicine, Mater Misericordiae University Hospital, Eccles St, Dublin 7
Email: [email protected]
References
1. Franquet T, Muller NL, Gimenez A, Guembe P, de La Torre J, Bague S. Spectrum of pulmonary aspergillosis: histologic, clinical, and radiologic findings. Radiographics : a review publication of the Radiological Society of North America, Inc. 2001 Jul-Aug;21:825-37.
2. Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest. 2002 Jun;121:1988-99.
3. Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: a meta-analysis. Clin Infect Dis. 2006 May 15;42:1417-27.
4. Kousha M, Tadi R, Soubani AO. Pulmonary aspergillosis: a clinical review. European respiratory review : an official journal of the European Respiratory Society. 2011 Sep 1;20:156-74.
5. Park CK, Jheon S. Results of surgical treatment for pulmonary aspergilloma. Eur J Cardiothorac Surg. 2002 May;21:918-23.
6. Abramson S. The air crescent sign. Radiology. 2001 Jan;218:230-2.