Introduction
There have been numerous papers on the quality, content and communication process involved in handing over patients at admission to or discharges from ICU and at change of a duty shift1-3. In anaesthesia there is a routine transition of care from an anaesthetist to the recovery room (PACU: Post Anaesthesia Care Unit) nurse. A recent review of literature identified 31 papers dealing with handovers in the postoperative period with many recommendations suggested. However, only 4 of these studies, all dealing with postoperative handover to ICU mainly in the paediatric population, introduced an intervention and assessed its impact on quality of handover or teamwork4. The Association of Anaesthetists of Great Britain and Ireland guidelines5 state that “the anaesthetist must formally handover care of a patient to a recovery room nurse or other appropriately trained member of staff. The anaesthetist is responsible for ensuring that this transfer is accomplished safely.” This ensures safety and continuity of care for patients. The document, however, fails to mention the essential content that this handover must contain. Despite best intentions, various activities in the dynamic recovery room environment distract from a smooth transfer of information and care. The information transfer process is usually informal, with the anaesthetist and nurses differing on the time and content of handover6.
In the AIMS study, 1 in 20 incidents recorded occurred during recovery7. Kluger and Bullock claimed that poor communication contributed to 14% of the 419 incidents8. The Closed Claims Study in the United States9 and Hines et al10 have cited recovery room mishap rates of 5-23.7%. This highlights the problem that exists and a potential area of improvement. The aim of our audit was to assess the quality of current anaesthetic handover to nurses in the recovery room and to evaluate the short term effect of a structured framework for transfer of information, on the quality of handover.
Methods
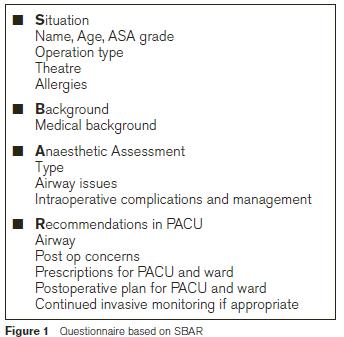
The audits were conducted in the recovery room of Beaumont Hospital, Dublin where the routine nurse: patient ratio is 2:1.The audits were registered with the hospital clinical governance and audit committee. A questionnaire based on the Situation Background Assessment and Recommendations (SBAR) system11,12 was formulated. Recovery nurses completed this questionnaire after the anaesthetist had handed over the patient and left the recovery. The responses were based on information voluntarily imparted by the anaesthetist. The anaesthetists were unaware of both the content of the questionnaire and timing of the audit. Following Audit A, the results were presented to the department and use of a structured framework, based on the SBAR, advised. We further suggested conducting handovers in recovery following a defined process “Connect, Observe, Listen, Delegate” (COLD) as recommended by Professor Mari Bottiet et al13. Educational sessions were in the form of an audiovisual presentation, electronic reminders, posters at hospital meetings and memory aid at recovery bays.
After an interval of one month, audit B, was conducted to assess change in quality of handover and subjective nurse assessment of satisfaction with handover process. To prevent operator bias, handovers were audited on randomly selected days. Pearson’s chi 2 test was applied and p<0.05 was taken as statistically significant. A difference of >10% was taken as clinically significant.
Results
Audits were conducted over a period of 2 months each (February 2012 to June 2012) at a month’s interval. To ensure that data was anonymous, patient demographics, transfer anaesthetists’ grade and the recording nurse’s identification were omitted.
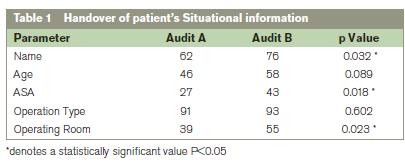
Situational data
In Audit A, more than 90% anaesthetists handed over information regarding type of surgery the patient had undergone which was similar in Audit B (p=0.62). 62% patients in audit A were handed over to the recovery nurses by name in audit A with a 14% increase in audit B which was statistically significant (p=0.032). Their age and ASA group were included in 12% (p=0.089) and 16% (p=0.018), respectively, of more handovers in audit B and 16% more anaesthetists included information regarding the operating room number (p=.033).
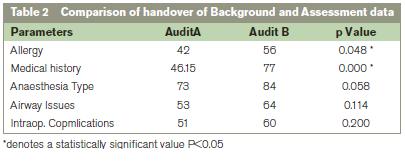
Background data
In audit A 42% of handovers included information on allergy status and 46% on medical background of patients. Compared to Audit A, 14% more anaesthetists mentioned allergy status (p=0.48) and 31% (p<0.001) more included medical background in audit B which were both statistically significant.
Assessment data
This included information regarding anaesthesia type, type of airway used, difficult airway issues and intraoperative complications. Nearly 11% more handovers included this information in Audit B compared to audit A. After educational sessions, there was an improvement of 15%, 13% and 9% in handover of information regarding intraoperative administration of antibiotics, antiemetics and fluids, respectively. Handover of analgesics administered intraoperatively, remained unchanged at 85%. These changes were, however, not statistically significant (see Table 2).
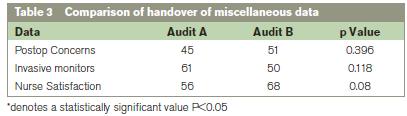
Recommendation data
Though, in audit B, 6% more anaesthetists verbally handed over advice regarding analgesia for the recovery room than in audit A, there was no change in the numbers handing over instructions regarding other drug therapy in recovery. Nurse satisfaction with the quality of handover improved from 56% in audit A to 68% in audit B, but was not statistically significant (p=0.08). 11% fewer anaesthetists issued verbal instructions regarding fate of invasive monitoring lines in audit B.
Discussion
Handovers have an important role to play in transfer of information regarding patients’ progress and maintaining continuity of care, organisation of care with respect to immediate post op care and a learning opportunity for all involved. Clinical handover is defined as “the transfer of clinical and professional responsibility of some or all aspects of care of a patient to another person or professional group on a temporary or permanent basis”14. Hence transfer of relevant information should be organised, quick, coherent and complete in 100% of handovers12. A recent publication from Boston, suggests that poor quality handovers may be responsible for a longer stay in recovery which in turn impacts on theatre effectiveness. This held true even when the authors corrected for pain intensity and severity of illness15. Smith et al had concluded in their paper7 that this important link in a patient’s care pathway was conducted in an informal manner despite the patient having been under close observation of an anaesthetist just minutes before transfer and while he may still be under residual effects of anaesthesia. Also “local negotiations”, where the senior recovery nurse made alternate arrangements to gather information and provide appropriate care rather than challenge an unsatisfactory standard of care were prevalent .
Recovery has a dynamic environment, plenty of distractions, a venue where both intra and inter professional handovers are the routine and has a high turnover of patients. Such a situation is fraught with errors arising from miscommunication or omission of information transfer. There are multiple guidelines for standards of post anaesthesia care but content of handovers has been a largely neglected part of training and assessment16. All the transferred information may not be necessarily recalled. Hence it is prudent on the part of the parties involved to not only ensure a smooth transfer of care, but also to stop and listen.
Audit A demonstrated that the quality of handover observed in our recovery room was in keeping with that reported in other publications. Anwari17 surveyed 276 patient handovers in a single centre in Riyadh. He assessed the handovers by assigning score for data, anaesthetists behaviour and nurse satisfaction. In his survey, 40% anaesthetists verbally reported the ASA status of the patient, 36% informed recovery nurses about premedication used and 64% about intra operative analgesia. 15% of anaesthetists in that survey informed nurses about course of surgery and complications during anaesthesia and 21% about the surgical procedure. 80% of anaesthetists gave clear post op instructions. Nearly half of the handovers were judged as satisfactory by the nurses. As in Anwari’s study, handover on intra operative analgesia was the most commonly included information at 85% of handovers in audits A and B. This most likely reflects anaesthetists’ attitude of responsibility for provision of analgesia. Clear instructions for post operative care in recovery were given regarding analgesia, antiemetics, fluids to be administered and O2 therapy in 70% , 61%, 52%,and 50% of handovers in audit A and remained largely unchanged in audit B. In audit A, nurse satisfaction with the handover, was in keeping with Anwari’s findings. With education, this improved to 68% which was not statistically significant although it is clinically significant. However, nurse satisfaction is subjective, hence, open to bias and influenced by various human factors such as interpersonal skills, habits and manners. Post education, there was significant increase in the handover of ASA grading and medical and allergy history. This may be the result of anaesthetist's concept of "important information" for appropriate care of patients.
Anaesthetists involved may become aware of the ongoing audit and change practice in the short term, thus introducing bias. An attempt was made to overcome this by random selection of days when handovers were audited. Since the repeat audit was undertaken after a short interval of a month, we cannot comment on long term validity of results. Furthermore, we did not attempt to look at the contribution of poor handovers towards incidents or length of stay in the recovery. It has been previously suggested that introducing a formal structure to the handover process would facilitate transfer of information. This in turn may reduce “adverse events” from lack of communication which in an Australian survey was found to have a 14% contribution towards “incidents” in recovery room9.
We introduced SBAR format for handover12 to lend a formal structure to handovers in the recovery. The repeat audit demonstrated a change in focus of information transfer to the situational, background and intra operative areas of the handover. Even though verbal handover of instructions for the ward showed a downward trend, recovery nurses were more satisfied with the information they received. We attribute this to presence of written post op instructions, which this audit did not include. Though we did not audit follow up on our suggestion of “COLD”, it could be another reason for increased nurse satisfaction. Audit B showed a trend towards improved transfer of information, but the numbers were far from the “ideal” 100%. Simulation based handover learning may have a role in improving handovers. Weinger et al reported that in 981 handovers, simulator based training resulted in a statistically significant improvement in handover to recovery nurses18. Handovers by participants who had received simulator based training were judged more effective. Kalmen et al19 got similar results from training medical students in the art of handovers in simulated inpatient settings. At present formal training in handovers for anaesthetists is sadly lacking.
We conclude that though anaesthesia is recognised as a safety conscious speciality, we do not recognise recovery handovers as an important link in the chain of safe care. In our opinion, introducing a formal structure to handovers, simulation based training and daily use of SBAR based handovers will ensure adequate transfer of information and continuity of care.
Correspondence: A Grover
Department of Anaesthesia, Beaumont Hospital, Beaumont Road, Dublin 9
Email: [email protected]
Acknowledgement
P Lohan (CNM, PACU, Beaumont hospital) and all PACU staff for their co-operation in data collection. P O’Kelly for his statistical advice. No funding was sought for this audit. No competing interests.
References
1. World Health Organization Patient safety solution: communication during patient handovers. http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution3.pdf (Accessed 16/01/2012)
2. Fletcher KEMM, Saint SM, Mangrulkar RSM: Balancing continuity of care with residents' limited work hours: defining the implications. Acad Med, 2005, 39–43
3. Li P, Stelfox HT, Ghali WA, A Prospective Observational Study of Physician Handoff for Intensive-Care-Unit-to-Ward Patient Transfers. The American Journal of Medicine: 2011; 124: 860–867
4. Segall N, Bonifacio AS, Schroeder RA, Barbeito A, Rogers D, Thomlow DK, Emery J, Kellum S, Wright MC, Mark J: On behalf of the Durham VA Patient Safety Centre of Inquiry. Can We Make Postoperative Patient Handovers Safer? A Systematic Review of the Literature Anesth Analg 2012; 115:102–15
5. Immediate post anaesthetic recovery.AAGBI, 2002 http://www.aagbi.org/publications/guidelines/docs/postanaes02 (accessed 16/01/2012). 6. Smith AF, Pope C, Goodwin D and Mort M. Interprofessional handover and patient safety in anaesthesia: observational study of handovers in the recovery room British Journal of Anaesthesia 101:332–7
7. Runciman WB, Sellen A, Webb RK, Williamson JA, Currie M, Morgan C, Russell WJ. The Australian Incident Monitoring Study. Errors, incidents and accidents in anaesthetic practice. Anaesth Intensive Care.1993; Oct 21:506-19
8. Kluger MT and Bullock MFM: Recovery room incidents: a review of 419 reports from the Anaesthetic Incident Monitoring Study (AIMS): Anaesthesia, 2002; 57, 1060-1066
9. Zeitlin GL. Recovery room mishaps in the ASA Closed Claims study. ASA Newsletter 1989; 53; 28-30
10. Hines R, Barash PG, Watrous G, and O’Connor T. Complications occurring in the postanesthesia care unit: a survey. Anesthesia and Analgesia 1992; 74: 503-9
11. Handover of responsibility for patients in the post anaesthetic care unit: Raising the Standard: A compendium of audit recipes (Second edition 2006) Royal College of Anaesthetists U.K.
12. Institute for Healthcare Improvement: SBAR technique for communication www.ihi.org/IHI/Topics/PatientSafety/Safety General/Tools (accessed 16/01/2012)
13. Interprofessional communication and team climate in complex clinical handover situations: issues for patient safety in the private sector FINAL REPORT April 2009
14. Safer Handover: Safer Patients. Australian Medical Association, 2006, 8
15. Bittner EA, George E, Eikermann M, Schmidt U: Evaluation of the association between quality of handover and length of stay in the post anaesthesia care unit: a pilot study. Anaesthesia 2012; 67:548-489
16. Vimlatia L, Gilsanzb F and Goldik Z: Quality and safety guidelines of post anaesthesia care Working Party on Post Anaesthesia Care (approved by the European Board and Section of Anaesthesiology, Union Europe ´enne des Me´ decins Spe´cialistes) European Journal of Anaesthesiology 2009; 26:715–72
17. Anwari JS. Quality of handover to the post anaesthesia care unit nurse: Anaesthesia 2002; 57,484-500
18. Weinger MB, Slagle JM, Kuntz A, Banerjee A, Schildcrout JS et al: Improving actual handover behaviour with a simulation-based training intervention. Proceedings of the Human Factors and Ergonomics Society Annual Meeting September 2010; vol. 54 no. 12 957-961
19. Klamen DL, Reynolds KL, Yale B, Aiello M: Students learning handovers in a simulated in-patient unit. Medical Education 2009; 43, 1097–1098