Introduction
The majority of respiratory tract infections (RTI’s) are self-limiting, and do not require antibiotic treatment3. A delayed prescription is given to the patient with the understanding that it is only to be used if specific symptoms worsen or if there is no improvement within a defined period of time. Use of a delayed antibiotic prescription has been suggested as a tool to reduce antibiotic usage, and could potentially have a positive impact in preventing antibiotic resistance4. A patient’s decision to fill the prescription and use the antibiotic may be influenced by how the delayed prescription is explained in the consultation5. Written information regarding the appropriate use of antibiotics could be used to improve patient education and may further reduce the number of prescriptions filled. The aim of the study was to examine the use of delayed prescriptions for RTI’s, and to determine if concurrently providing the patient with an information leaflet on the appropriate use of antibiotics in RTI’s and their potential side effects influences the rate of antibiotic use.
Methods
This was an intervention trial design. Ethical approval was obtained from the TCD/HSE GP Training Scheme Ethics Committee. The control group (n = 69) were given a delayed prescription for RTI, and the intervention group (n = 46) were given a delayed prescription with an information leaflet outlining role of antibiotics in RTI’s, indications for use and potential side effects. Cases were included on the basis of their serial presentation at a Teaching Practice with four doctors. Basic demographic information was recorded for each patient given a delayed prescription. Data for the control group was recorded over a 5 week period and then the intervention group over a consecutive 5 week period. All patients presenting with RTI during the defined periods were included in the study. Verbal consent was obtained during the consultation. Data was collected by the treating Doctor in the practice, including current patient contact details. Each patient was subsequently contacted by telephone at 10-14 days post consultation, and asked if they had used the antibiotic on the delayed prescription.
Results
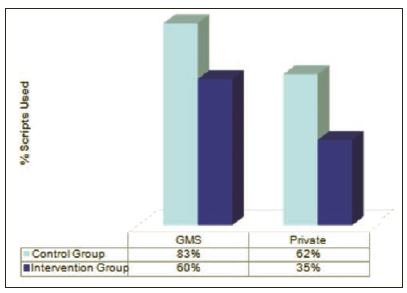
A total of 115 delayed prescriptions were presented; 69 in the control group (delayed prescription alone) and 46 in the intervention group (delayed prescription and information sheet). Both the proportion of fee paying versus primary care service eligible patients (65:50), together with the range of patient age indicated a robust degree of case mix, typical and representative of routine General Practice consulting. In the control group, 72% of patients used the antibiotic, and in the intervention group, 43% indicated they used the antibiotic, which difference was statistically significant (p = 0.0018), indicating that use of an information sheet with the delayed prescription was effective in very significantly reducing use of antibiotics. This effect was most evident among fee paying patients, who were less likely to use the antibiotic in both groups (Figure 1).
Figure 1: Control Group vs Intervention Group
Discussion
Appropriately reducing the use of antibiotics for self limiting viral infections continues to be an important objective in routine prescribing. This study observes the impact of a simply designed practice information sheet on when it is appropriate to use an antibiotic, what steps should be taken to self care an uncomplicated viral RTI together with clear information on common negative consequences of inappropriate antibiotic use. Despite the modest sample size, a clear and significant reduction in antibiotic use is evident in the intervention group. This study was carried out in a Training Practice, where antibiotic prescribing is more likely to be conservative6, which renders the reduction in antibiotic use even more significant. This study demonstrates that use of an accompanying information leaflet is highly effective at reducing the use of antibiotics in delayed prescribing. It supports the uniform use of such leaflets based on a modest study utilising an intervention trail methodology on a small sample. It is proposed to conduct a larger block randomised control trial in order to confirm the approach can be generalised.
Correspondence: B O’Shea
GP Training Scheme, TCD Teaching Centre, AMNCH, Tallaght, Dublin 24
Email: [email protected]
References
1. Antibiotic Prescribing: A challenge for Primary Care. MeReC National Prescribing Bulletin Vol 11 No 5 2000, www.npc.nhs.uk/merec/other_non.../merec_bulletin_vol11_no12.pdf.
2. Harnden A, Perera R, Brueggemann AB, Mayon White R, Crook D, Thomson A, Mant D. Respiratory Infections for which general practitioners consider prescribing an anti biotic: a prospective study. Arch Dis Childhood 2007; 92: 594-597.
3. Jochen WL, Boumans D, Lardinois R, Gonzales R, Hopstaken RM, Butler C, Dinant G. Public beliefs on antibiotics and respiratory tract infections. British Journal of General Practice 2007; 57:942-944
4. Strategy for Control of Antibiotic Resistance in Ireland 2011. Health Service Executive Health Protection Surveillance Centre (www.hpsc.ie/A-Z/MicrobiologyAntimicrobialresistanceinIrelandSARI/com)
5. Little P. Delayed Prescribing of antibiotics for upper respiratory tract infections. BMJ 2005 Vol 331 p 301 (editorial).
6. Lo YYC, Lam CLK, Mercer SW, Fong DYT. Does vocational training in family medicine have an impact on antibiotic prescribing pattern? Family Practice 2011; 28:56-62.
7. Why no antibiotic? http://www.patient.co.uk/health/Antibiotics-Why-No-Antibiotic?.html