|
|
|
|
|
|
|
|
Nnamdi Nkire,Ugochukwu Obiora Ekwegbalu,chinedu iro,John O'Connor
|
|
|
Ir Med J. 2013 Jan;106(1):21-2
N Nkire, UO Ekwegbalu, C Iro, J O'Connor
Drug Treatment Centre Board, Pearse St, Dublin 2
Abstract
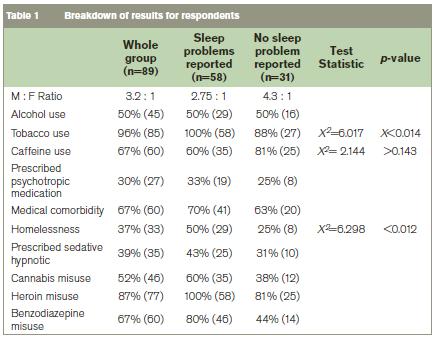
This study evaluated subjective reports of sleep difficulties in patients attending a designated consultant in The Drug Treatment Centre Board (DTCB). 89 patients consented to participate representing a 51% response rate. Approximately 65% complained of sleep difficulties. All those who complained of sleep problems had multiple sleep difficulties. About 37% reported six month duration of complaints at time of assessment. There was a significant association between reports of sleep difficulties with homelessness (Pearson’s X2= 6.298, p< 0.012), cigarette smoking (Pearson’s X2=6.017, p<0.014) and day time sleep (Pearson’s X2=3.920, p<0.048). Sleep problems are common amongst patients attending our opioid replacement treatment programme. The present study suggests measures to ensure a holistic management of complaints.
|
|
Introduction
Problems with sleep are common in the general population. They range from 4 – 50% depending on the setting or definition1. Sleep problems may arise from general medical conditions or mental disorder. Indeed high rates of sleep difficulties have been reported in the psychiatric population, and substance using cohorts2. Disturbed sleep architecture has been observed during induction, maintenance and withdrawal of opioids. Chronic opioid use has been associated with Central Sleep Apnoea (CSA) with reports that as much as a third of stable methadone maintenance patients have CSA3. Additionally, Obstructive Sleep Apnoea (OSA) is common in this group of patients especially amongst patients who drink heavily4.
Although it has been established that alcohol may impair sleep, a study of over 300 addiction physicians found that sedatives were prescribed to less than a third of their patients who were alcohol dependent and complained of insomnia5. Failure to adequately manage insomnia in patients with addiction problems may in itself pose a risk of relapse of addiction. Bearing this in mind, and considering that the DTCB is the foremost addiction treatment centre in Ireland we sought to evaluate reports of sleep difficulties in patients attending a designated consultant at the DTCB.
Methods
Patients attending JJO’s clinic at the DTCB were approached for inclusion in the study. Patients included were aged 18 years and above and all were on methadone maintenance treatment for opioid addiction. The study involved the completion of a self-report questionnaire (available on request) designed by the authors. This exercise was carried out over a one month period. Variables examined included demographic details, sleep complaints (presence of difficulties falling asleep and/or sleeping through), smoking, medical and psychiatric problems and drug and medication use. The study received Local Ethics and Research Committee approval.
Results
Of the 175 consecutive patients approached 89 completed questionnaires with a response rate of 51%. Results are summarised in table 1. About 96% (85) of the cohort were Irish nationals, 76% (79) were males, (87% (77) were single, 93% (83) were unemployed and 37% (33) were homeless. Mean age was 40 years. Reports of sleep difficulties were approximately three times more common amongst male respondents compared with females. Approximately 65% (58) of respondents reported sleep difficulties. Of these, all reported initial insomnia, 93% (54) reported middle insomnia, and 66% (38) reported terminal insomnia. All those who complained of sleep problems reported multiple sleep difficulties with the commonest combination (60%) being a combination of difficulties with the three phases (initial, middle and terminal insomnia). Approximately two-third of patients reported sleeping for 6 hours or less.
Approximately 96 % of the cohort reported smoking cigarettes and of these, 68% reported sleep difficulties (Pearson’s X2=6.017, p<0.014). Homelessness was twice as common in those reporting sleep difficulties (50%) versus no sleep difficulties (25%) (Pearson’s X2=6.298,p< 0.012). Approximately 41% of the cohort admitted day time sleep and there was a significant report of night time sleep difficulties in the cohort (Pearson’s X2=3.920, p<0.048). There was no significant association between complaints of sleep difficulties and prescription of sedative medications, caffeine use, alcohol use or sharing of sleeping area.
Discussion
Sleep difficulties in this study was broadly defined as difficulty getting to sleep, staying asleep, waking early, and sleeping less than 6 hours at night. The high rate of reported sleep difficulties in our cohort was generally in line with that of other studies1. Alcohol use was evenly spread amongst those reporting or denying sleep difficulties. The potential for sleep complaints to progressively worsen and become chronic may have a negative impact on outcomes6. Although it is generally accepted that insomnia is more common in females than males7, our study showed proportionately more subjective reports of insomnia amongst males than females. This finding may perhaps be explained by the pattern of substance use of male respondents. Sleep difficulties persisted despite the fact that 43% of those complaining of sleep problems took hypnotics. As such problems like homelessness, smoking and day time sleep identified as affecting sleep can form additional foci of treatment for people with substance use and sleep difficulties. Provision of appropriate accommodation and daytime vocational activities may serve not only to rehabilitate patients but may also positively influence sleep. OSA, a major cause of daytime sleepiness in the general population poses a significant risk in this population group4. Therefore identifying and treating OSA sufferers will reduce morbidity. This study was based on a self-report as such subject to the bias of over reporting.
Correspondence: N Nkire
Drug Treatment Centre Board, Pearse St, Dublin 2
Email: [email protected]
Acknowledgements
D Daly, Nursing staff and General Assistants at the Drug Treatment Centre Board
References
1. Neumann T, Neuner B, Weib-Gerlach E, Spies C. Complaints about sleep in trauma patients in an emergency department in respect to alcohol use Alcohol and Alcoholism 2008;43: 305 - 313
2. Conroy D, Arnedt JT, Brower KJ. Insomnia in patients with addictions: A safer way to break the cycle. Fight relapse by improving sleep with non addictive agents and behavior therapy. Curr Psychiatr 2008; 7: 97-109
3. Wang D, Teichtahi H. Opioids, sleep architecture and sleep-disordered breathing. Sleep Med Rev 2007; 11: 35 – 46
4. Sharkey KM, Kurth ME, Anderson BJ, Corso RP, Millman RP, Stein MD. Obstructive sleep apnea is more common than central sleep apnea in methadone maintenance patients with subjective sleep complaints. Drug Alcohol Depend 2010; 108: 77-83
5. Friedmann PD, Herman DS, Freeman S, Lemon SC, Ramsey S, Stein MD. Treatment of sleep disturbance in alcohol recovery: a national survey of addiction medicine physicians. J Addict Dis 2003; 22: 91- 103
6. Asaad TA, Ghanem MH, Abdel S, Afaf M, El-Habiby MM. Sleep profile in patients with chronic opioid abuse: A polysomnographic evaluation in an Egyptian sample. Addic Disord Treat 2011; 10: 21-28
7. Voderholzer U, Al-Shajlawi A, Weske G, Feige B, Reimann D. Are there gender differences in objective and subjective sleep measures? A study of insomniacs and healthy controls. Depress Anxiety 2003;17: 162- 172
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|