|
|
|
|
|
|
|
|
Ferdia Bolster,Lawler Leo P,G McEntee
|
|
|
Ir Med J. 2013 Feb;106(2):56-7
F Bolster, LP Lawler, G McEntee
Mater Misericordiae University Hospital, Eccles St, Dublin 7
Abstract
Annular Pancreas (AP) is a developmental disorder uncommonly suspected in adults. We report a case presenting with signs and symptoms of progressive gastric outlet obstruction. The diagnosis was suggested on pre-operative imaging and confirmed at laparotomy where the patient was successfully treated with a bypass procedure.
|
Case Report
After a recent episode of pancreatitis a 40-year-old man presented with increasing nausea, early satiety, post prandial fullness, vomiting and weight loss of approximately 7 kilograms over 2 months. Examination revealed recent weight loss and mild epigastric tenderness. His laboratory results were all within normal limits aside from an initial hyponatraemic hypochloraemic metabolic alkalosis which was corrected. An OGD showed mild inflammation and a tight duodenal stenosis at D1/2. Biopsies revealed normal intestinal mucosa. Endoscopic ultrasound was unsuccessful due to the degree of stenosis and a naso-jejunal feeding tube was placed.
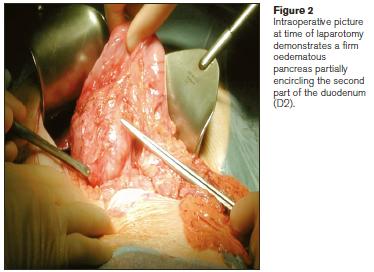
A CT confirmed gastric outlet obstruction (Figure 1) and a concentrically thickened and oedematous D2 stricture. MRCP was performed which showed pancreatic tissue and pancreatic duct partially encircling the duodenum and a suspected diagnosis of incomplete AP was made. The patient underwent an exploratory laparotomy (see Fig. 2) where a firm oedematous pancreas was found to be partially encircling the D2 concordant with imaging findings. Multiple biopsies revealed chronic inflammation with no evidence of malignancy. A gastrojejunostomy bypass was performed and the patient underwent an uneventful postoperative recovery.

Discussion
Annular Pancreas is an uncommon developmental abnormality of the pancreas which was first described by Tiedeman at time of autopsy in 1818. It was first termed “annular” by Ecker in 1862, so called because it forms a “ring” or “annulus” of pancreatic tissue partially or completely surrounding the duodenum.1,2 The true incidence of annular pancreas(AP) is unknown, but is estimated to be approximately 1 in 2000 based on autopsy, imaging and endocsopic series.3 Several theories exist to describe the embryological development of AP and the 2 best known are those of Baldwin and Lecco. Both centre on the failure of the ventral anlage to rotate and fuse in the 7th week of gestation leaving a rest of tissue on the opposite side of the duodenum forming a ring4,5. Partial annular anatomy reflects the spectrum of anomalies possible. Patients symptomatic from AP present in 2 main age groups3. Neonates usually present in the first few days of life with gastric outlet obstruction frequently detected on prenatal screening using the “double bubble” sign and often associated congenital abnormalities such as cardiac defects, intestinal atresia, biliary anomalies, tracheooesophageal fistulae, intestinal malrotation and trisomy 21.3 It is estimated that only 10% of all adult AP are symptomatic6. These adults present with some combination of pain, jaundice, and vomiting in the 4th decade of life perhaps precipitated by pancreatitis which has an increased prevalence in AP. There is an association with pancreatic divisum and also with hepatobiliary malignancy (up to 11%) which should be excluded preoperatively.3
The preoperative diagnosis of AP is often difficult and may only be made definitively at surgery in up to 40% of cases.7 Today the diagnosis is usually made by some combination of CT, MR and MRCP with the complimentary use of ERCP and EUS6,8. Together these modalities can assess the foregut, biliary anatomy and pancreatic tissue. The mainstay of treatment for symptomatic AP is surgery with bypass of the obstruction being the preferred procedure. Resection or division of the annulus should not be attempted as complications include pancreatic fistula, pancreatitis and persistence of the obstruction due to intrinsic duodenal luminal narrowing and fibrosis.3
Correspondence: F Bolster
Department of Radiology, Mater Misericordiae University Hospital, Eccles St, Dublin 7
Email: [email protected]
References
1. Tieddmann F. Uber die Verschiedenheiten des Ausfuhrungsgangs der Bauchspeicheldruse bei den Menschen und Saugetieren. Dtsch Arch Physiol 1818; 4:403.
2. Ecker A. Bildungsfchler des pancreas und Herzens. Z Rat Med 1862; 14: 354.
3. Zymonski NJ, Sandoval JA, Pitt HA, Ladd AP, Fogel EL, Mattar WE,
Sandrasegaran K, Amrhein DW, Rescorla FJ, Howard TJ, Lillemoe KD, Grosfeld JL.
Annular Pancreas:dramatic differences between children and adults. J Am Coll Surg 2008:206:1019-1025.
4. Lecco TM. Zur Morphologie des Pankreas annulare. Sitzungb Akad \wissensch 1910; 119:391-406
5. Balwin WA. A specimen of annular pancreas. Anat Rec 1910;4:299-304
6. Mortelé KJ, Rocha TC, Streeter JL, Taylor AJ.
.Multimodality Imaging of Pancreatic and Biliary Congenital Anomalies. Radiographics 2006:26;715-731
7. Urayama S, Kozarek R, Ball T, Brandabur J, Traverso L, Ryan J, Wechter D. Presentation and treatment of Annular Pancreas in an adult population. Am J Gastroenterology 1995; 90 :995-9.
8. Sandrasegaran K et al. Annular Pancreas in Aduls. AJR 2009;193:455-460
|
|
|
|
Author's Correspondence
|
|
No Author Comments
|
|
|
Acknowledgement
|
|
No Acknowledgement
|
|
|
Other References
|
|
No Other References
|
|
|
|
|